-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
The global spread of carbapenem-resistant Enterobacteriaceae (CRE) poses a serious threat to public health systems
.
Enterobacteriaceae mainly acquire carbapenemases for drug resistance, of which Klebsiella pneumoniae carbapenemases (KPCs) are the most prevalent
.
KPCs-producing CREs have spread worldwide, often accompanied by multidrug resistance, and are a major cause of increased morbidity and mortality from hospital-associated infections (HAIs)
.
To make matters more difficult, KPCs-producing CREs often show low-level drug resistance in routine laboratory screening, leading to misdiagnosis or missed diagnosis and thus affecting the therapeutic effect
.
While unstable gene amplification has been identified as a key factor contributing to the underestimation of resistance in clinical strains, to date, the precise mechanism of carbapenem resistance mediated by blaKPC-2 amplification, as well as combined The therapeutic evaluation of medication for this resistance remains blank
.
The team of Feng Jie from the Institute of Microbiology, Chinese Academy of Sciences revealed through epidemiological analysis earlier that the pathogenic bacteria Escherichia coli ST131 caused its large-scale epidemic in hospitals by obtaining different types of plasmids carrying the blaKPC-2 gene (Front Microbiol, 2020)
.
Recently, the team conducted in-depth research on one of the treatment failure cases and found that a strain of E.
coli carrying the blaKPC-2 gene can rapidly become a highly resistant phenotype after exposure to sublethal antibiotics, which explains the patient's Key cause of death after antibiotic treatment
.
Further studies found that the occurrence of high drug resistance is due to the dynamic and unstable expansion of multidrug resistance (MDR) regions including the blaKPC-2 gene mediated by the insertion sequence IS26, a mechanism that helps bacteria to escape The challenge of carbapenems is also an important strategy for CRE to escape laboratory in vitro resistance detection, which in turn affects the use and efficacy of antibiotics in clinical applications
.
In addition, the team evaluated the in vitro therapeutic effect of the combination drug strategy.
The experiment found that inappropriate drug combination not only could not prevent the expansion of multi-drug resistance regions, but instead increased the rate of gene amplification to a certain extent, making subsequent treatment more efficient.
difficult, which has important guiding significance for clinical medication
.
The above research provides a new perspective for bacterial carbapenem resistance, and the results have been published in the journal mBio (DOI: 10.
1128/mbio.
03340-21), entitled "IS26 veers genomic plasticity and genetic rearrangement toward carbapenem hyperresistance under sublethal" antibiotics”
.
Wei Dawei, a doctoral student in Feng Jie's research group from the Institute of Microbiology, Chinese Academy of Sciences, and Huang Naiqi, professor of Shantou University, are the co-first authors, and researcher Feng Jie is the corresponding author
.
The research was supported by the National Natural Science Foundation of China
.
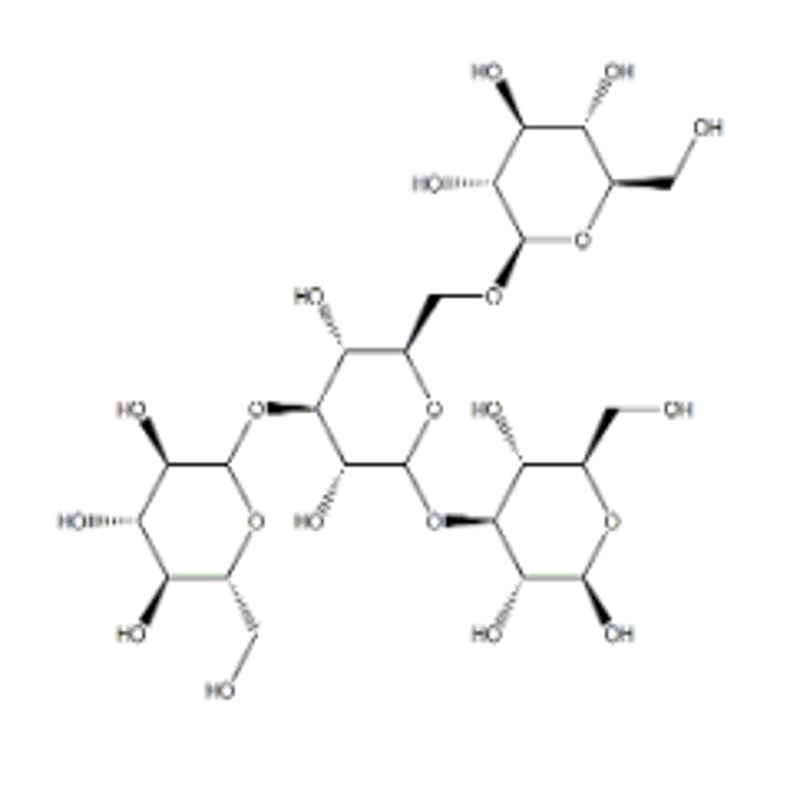
Figure 1 The strains rapidly increase carbapenem resistance through gene amplification after exposure to sublethal antibiotics (Note: the cover is a schematic diagram)