-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*Only for medical professionals to read and refer to these types of drugs should be used with caution! According to the World Health Organization’s International Agency for Research on Cancer (IARC), colorectal cancer has risen to the third most common cancer after breast and lung cancer in 2020
.
The incidence of colorectal cancer in China is also on the rise.
Just last year, the number of new cases of colorectal cancer in China was as high as 560,000 [1]
.
Moreover, most colorectal cancers are already in the middle and advanced stages when they are diagnosed, and the effect is not good [2]
.
Facing the severe form of colorectal cancer with both high morbidity and mortality rates worldwide, and still rising, it can be said that, compared with passive treatment after cancer, active prevention and timely screening of colorectal cancer are improving patients The clinical outcome can bring more far-reaching significance
.
These 7 drugs may prevent colorectal adenoma.
The Chinese Society of Gastroenterology of the Chinese Medical Association has issued relevant guidelines for the prevention of colorectal cancer [2] (hereinafter referred to as "China Guidelines").
The guidelines point out that these 7 drugs may be preventive Occurrence of colorectal adenoma
.
NSAIDs such as aspirin and COX-2 inhibitors can reduce the initial and recurrence of colorectal adenomas, but there are potential adverse reactions
.
Folic acid intervention can prevent the occurrence of sporadic colorectal adenomas
.
Vitamin D intake and circulating hydroxyvitamin D levels are negatively related to the occurrence of colorectal adenoma to a certain extent
.
Calcium has the effect of reducing the recurrence of colorectal adenomas
.
Vitamin D has a certain preventive effect on the recurrence of colorectal adenoma; the combined application of calcium and vitamin D can prevent the recurrence of colorectal adenoma.
.
Metformin may have the effect of preventing the recurrence of adenomas, and more research is needed to verify it
.
Among these seven drugs, only two are recommended by AGA.
The only drugs recommended by AGA for the prevention of colorectal cancer are aspirin and metformin
.
1.
Aspirin ■ The AGA guidelines and regulations have a general risk of colorectal cancer, and people who meet the following conditions should use low-dose aspirin to reduce the incidence and mortality of colorectal cancer: ①Age less than 70 years old, and a life expectancy of at least 10 years
.
②The 10-year cardiovascular disease risk is at least 10%
.
③Patients with non-high-risk bleeding risk
.
In addition, for people with a history of colorectal cancer, clinicians may also consider using aspirin to reduce the recurrence rate of colorectal cancer
.
■ Recommended background Aspirin and non-aspirin (NSAIDs) mainly exert their anti-tumor effects by inhibiting the activities of cyclooxygenase COX-1 and COX-2
.
Metadata from 4 cardiovascular disease prevention trials (n=14033) found that taking 75-1200 mg aspirin daily can reduce the cumulative mortality of colorectal cancer by 33% (RR, 0.
67; 95% CI, 0.
52-0.
86) ) [3]
.
However, the protective effect of aspirin will only become apparent after 10-20 years of follow-up
.
The impact of aspirin dose is not clear, but longer duration of treatment (>5 years) may provide greater protection [4]
.
However, these early trials mainly recruited individuals in their early 60s who are at high risk of cardiovascular disease
.
For patients who have been diagnosed with colorectal cancer, a meta-analysis found that the use of aspirin can improve overall survival (HR, 0.
84; 95% Cl, 0.
75-0.
94)
.
However, this effect seems to be limited to individuals with PIK3CA gene mutations and COX-2 expressing tumors [5]
.
2.
Metformin ■ AGA Guidelines Regulations For patients with type 2 diabetes, clinicians may consider using metformin to prevent colorectal tumors
.
For patients with colorectal cancer and type 2 diabetes, clinicians may consider using metformin to reduce mortality
.
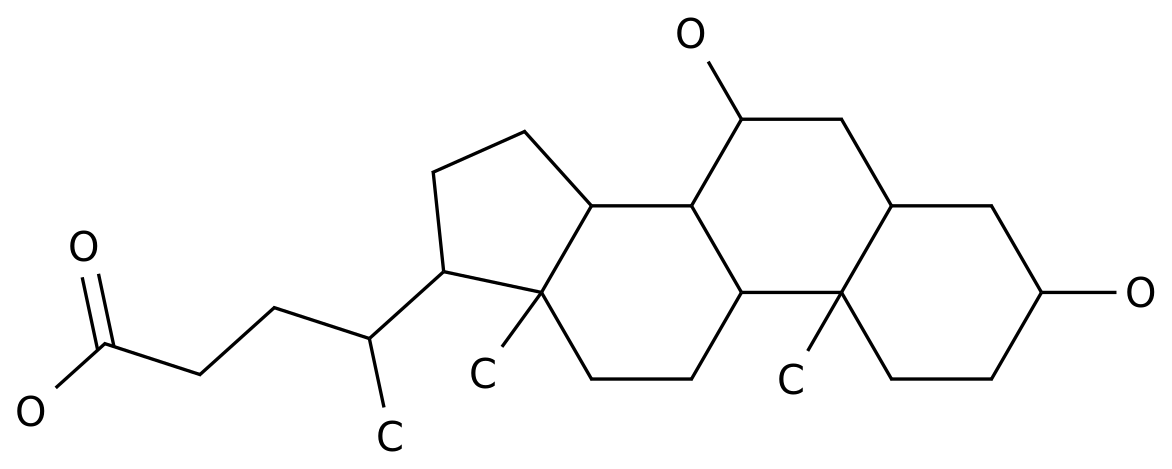
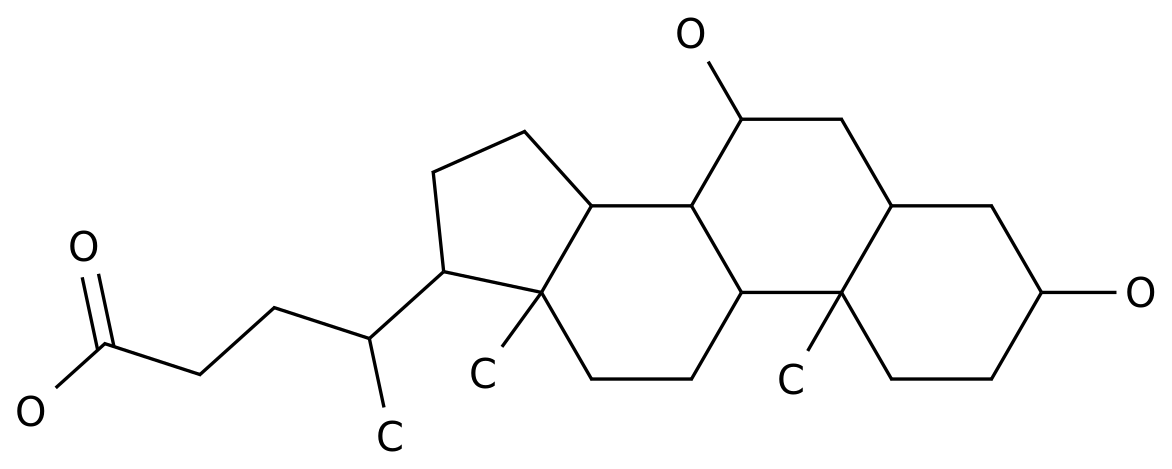
■ Recommended background Metformin is a biguanide anti-diabetic drug that can reduce the levels of insulin and insulin-like growth factor 1 in the blood that promote cell proliferation
.
In addition, it can directly activate the AMPK pathway and inhibit the proliferation of colon cancer cells [6]
.
A meta-analysis of 14 observational studies (n=459607) found that patients with type 2 diabetes who used metformin had a 27% reduction in the incidence of colorectal cancer compared with patients who did not use metformin (including those who used other treatments) (OR, 0.
73; 95% CI, 0.
62–0.
86) [7]
.
We know that the complete process of polyp carcinogenesis is "small polyps→adenoma→high-grade neoplasia→colorectal cancer"
.
So, where does metformin start its blocking effect? A meta-analysis of 5 observational studies (n=19730) found that metformin reduced the risk of adenoma in patients with type 2 diabetes by 20% (OR, 0.
80; 95% CI, 0.
71–0.
90)
.
Therefore, the blocking of the onset of colorectal cancer by metformin has already begun at least from the "polyp-adenoma" road
.
However, the editor here reminds everyone that although metformin is good, it is only suitable for the prevention of diabetic patients! It is not suitable for ordinary people who have no disease or disaster.
.
.
Except for aspirin and metformin which are recommended by AGA, the other 5 drugs are not recommended for the following reasons: 1.
Other non-aspirin NSAIDs drugs ■ AGA guidelines regulations due to non- Aspirin-like NSAIDs have a higher risk of cardiovascular and gastrointestinal adverse events.
Therefore, for people with a general risk of colorectal cancer, clinicians are not recommended to use these drugs
.
■ Recommended background.
In the past, two trials explored the effect of COX-2 inhibitors on the recurrence of adenomas [8-9].
However, due to the increased risk of cardiovascular events caused by COX-2 inhibitors, both studies were forced to terminate early
.
For non-selective non-steroidal anti-inflammatory drugs, gastrointestinal toxicity (peptic ulcer, gastrointestinal bleeding) is the main risk, and the increase in risk is related to the dose of the drug
.
2.
Calcium or Vitamin D ■ AGA Guidelines Regulations Clinicians should not use calcium or vitamin D (alone or in combination) to prevent colorectal tumors
.
■ Recommended background 1.
Calcium Calcium is an essential nutrient for the human body and has a variety of biochemical functions
.
For a long time, it has been believed that calcium can inhibit cell proliferation by binding to harmful free fatty acids and bile acids in the intestine, thereby preventing the occurrence of colorectal cancer [10]
.
Is it true? In fact, this point is full of controversy
.
Many observational studies have linked dietary intake and/or additional calcium supplementation with a reduction in the risk of colorectal cancer [11-13]
.
One of the largest studies was the 2016 analysis of nurse health studies and health professionals follow-up studies.
The study reached three key conclusions [14]: higher calcium intake and lower results The risk of rectal cancer is related (RR, 0.
78; 95% CI, 0.
65–0.
95); the relationship between calcium intake and the risk of colorectal cancer seems to be dose-dependent; dietary calcium intake and additional calcium supplementation have effects on colorectal cancer There does not seem to be a difference in the degree of reduction in morbidity
.
Based on these data, American Cancer Research even publicly stated that calcium supplements can reduce the risk of colorectal cancer [15]
.
However, the results of a recent larger randomized study suggest that calcium supplementation is not beneficial for the prevention of adenomas [16]
.
Some follow-up studies have also found that calcium supplementation is associated with an increased risk of sessile serrated polyps (RR, 2.
66; 95% CI, 1.
44–4.
89) [17]
.
More seriously, high calcium intake can increase the risk of prostate cancer [13], and excessive use of calcium supplements can also lead to nephrotoxicity, hypercalcemia and other metabolic abnormalities
.
2.
Vitamin D There is evidence that vitamin D has anti-proliferative effects in various tissues in the body (including colon).
In addition, the lack of vitamin D is also related to the occurrence of colorectal cancer
.
Most importantly, vitamin D has long been widely used as a dietary supplement worldwide and is relatively safe
.
However, many observational studies have investigated the association between vitamin D supplementation and the incidence of colorectal cancer or adenoma, and have not produced consistent results [18-26]
.
3.
Folic acid ■ AGA guidelines and regulations clinicians should not use folic acid to prevent colorectal tumors
.
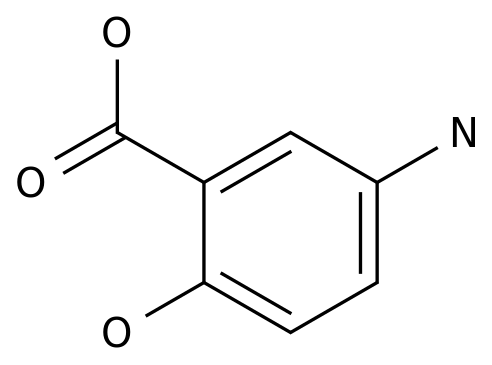
■ Recommended background Folic acid (vitamin B9) is an essential nutrient that has many important functions in the body
.
There is evidence that folic acid can inhibit the occurrence of colorectal cancer through a variety of mechanisms, including maintaining DNA synthesis and repair
.
According to nurse health research and follow-up research reports of health professionals, long-term intake of large amounts of folic acid is negatively associated with the risk of colorectal cancer (RR, 0.
69; 95% CI, 0.
51-0.
94) [27]
.
However, a large multicenter trial in the United States (n=1021) found that folic acid was associated with an increased risk of advanced adenoma and multiple adenoma [28]
.
In addition, in the folic acid group, the risk of cancers other than colorectal cancer also increased, especially prostate cancer [29]
.
4.
Statins ■ AGA Guidelines Regulations For people at general risk of colorectal cancer, clinicians should not use statins to prevent colorectal tumors
.
For people with a history of colorectal cancer, clinicians should not use statins to reduce mortality
.
■ Recommended background Statins are usually widely used in the treatment of hypercholesterolemia and cardiovascular diseases
.
The drug has a variety of anti-proliferative properties and inhibits the biosynthesis of cholesterol, which plays a key role in the progression of several cancers including colorectal cancer [30]
.
The effect of statins on the chemoprevention of colorectal tumors is currently unclear
.
Therefore, statins should not be used to prevent colorectal tumors at this time
.
References: [1] International Agency for Research on Cancer.
Late stglobal cancer data: Cancer burden rises to 19.
3 million new cases and 10.
0 million cancer deaths in 2020[EB/OL].
[2021-01-10].
https://www.iarc.
fr/faq/latest-global-cancer-data-2020-qa/.
[2] Chinese Medical Association Gastroenterology Branch (CSGE), Chinese Medical Association Gastroenterology Branch Cancer Cooperation Group.
China Colorectal Cancer Prevention Consensus (2016, Shanghai).
Chinese Journal of Digestion, 2016, 36(11): 721 -733.
[3]Chubak J.
Kamineni A.
Buist DSMet al.
Aspirin use for the prevention of colorectal cancer:an updated systematic evidence review for the USPreventive Services Task Force.
USPreventive Services Task Force,Rockville,MD2015.
[4]Rothwell PMWilson M.
Elwin CEet al.
Long-term effect of aspirin on colorectal cancer incidence and mortality:20-year follow-up of five randomised trials.
Lancet.
2010;376:1741-1750.
[5]Li P.
Wu H.
Zhang H.
et al.
Aspirin use after diagnosis but not prediagnosis improves established colorectal cancer survival: a meta-analysis.
Gut.
2015;64:1419-1425.
[6]MargaretE, RichardRS.
Liver directed the rapies in metastatic colorectal cancer[J].JGastrointestinalOncol, 2014, 5(5): 374-387.
[7]Peter S.
Liang,Aasma Shaukat,Seth D.
Crockett.
AGA Clinical Practice Update on Chemoprevention for Colorectal Neoplasia:Expert Review.
Clinical Gastroenterology and Hepatology.
DOI:https://doi.
org/10.
1016/j.
cgh.
2021.
02.
014.
[8]Bresalier RSSandler RSQuan H.
et al.
Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial.
N Engl J Med.
2005;352:1092-1102.
[9]Solomon SDMcMurray JJPfeffer MAet al.
Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention.
N Engl J Med.
2005;352:1071-1080.
[10]Algire C.
Amrein L.
Zakikhani M.
et al.
.
The incidence of colorectal cancer in China is also on the rise.
Just last year, the number of new cases of colorectal cancer in China was as high as 560,000 [1]
.
Moreover, most colorectal cancers are already in the middle and advanced stages when they are diagnosed, and the effect is not good [2]
.
Facing the severe form of colorectal cancer with both high morbidity and mortality rates worldwide, and still rising, it can be said that, compared with passive treatment after cancer, active prevention and timely screening of colorectal cancer are improving patients The clinical outcome can bring more far-reaching significance
.
These 7 drugs may prevent colorectal adenoma.
The Chinese Society of Gastroenterology of the Chinese Medical Association has issued relevant guidelines for the prevention of colorectal cancer [2] (hereinafter referred to as "China Guidelines").
The guidelines point out that these 7 drugs may be preventive Occurrence of colorectal adenoma
.
NSAIDs such as aspirin and COX-2 inhibitors can reduce the initial and recurrence of colorectal adenomas, but there are potential adverse reactions
.
Folic acid intervention can prevent the occurrence of sporadic colorectal adenomas
.
Vitamin D intake and circulating hydroxyvitamin D levels are negatively related to the occurrence of colorectal adenoma to a certain extent
.
Calcium has the effect of reducing the recurrence of colorectal adenomas
.
Vitamin D has a certain preventive effect on the recurrence of colorectal adenoma; the combined application of calcium and vitamin D can prevent the recurrence of colorectal adenoma.
.
Metformin may have the effect of preventing the recurrence of adenomas, and more research is needed to verify it
.
Among these seven drugs, only two are recommended by AGA.
The only drugs recommended by AGA for the prevention of colorectal cancer are aspirin and metformin
.
1.
Aspirin ■ The AGA guidelines and regulations have a general risk of colorectal cancer, and people who meet the following conditions should use low-dose aspirin to reduce the incidence and mortality of colorectal cancer: ①Age less than 70 years old, and a life expectancy of at least 10 years
.
②The 10-year cardiovascular disease risk is at least 10%
.
③Patients with non-high-risk bleeding risk
.
In addition, for people with a history of colorectal cancer, clinicians may also consider using aspirin to reduce the recurrence rate of colorectal cancer
.
■ Recommended background Aspirin and non-aspirin (NSAIDs) mainly exert their anti-tumor effects by inhibiting the activities of cyclooxygenase COX-1 and COX-2
.
Metadata from 4 cardiovascular disease prevention trials (n=14033) found that taking 75-1200 mg aspirin daily can reduce the cumulative mortality of colorectal cancer by 33% (RR, 0.
67; 95% CI, 0.
52-0.
86) ) [3]
.
However, the protective effect of aspirin will only become apparent after 10-20 years of follow-up
.
The impact of aspirin dose is not clear, but longer duration of treatment (>5 years) may provide greater protection [4]
.
However, these early trials mainly recruited individuals in their early 60s who are at high risk of cardiovascular disease
.
For patients who have been diagnosed with colorectal cancer, a meta-analysis found that the use of aspirin can improve overall survival (HR, 0.
84; 95% Cl, 0.
75-0.
94)
.
However, this effect seems to be limited to individuals with PIK3CA gene mutations and COX-2 expressing tumors [5]
.
2.
Metformin ■ AGA Guidelines Regulations For patients with type 2 diabetes, clinicians may consider using metformin to prevent colorectal tumors
.
For patients with colorectal cancer and type 2 diabetes, clinicians may consider using metformin to reduce mortality
.
■ Recommended background Metformin is a biguanide anti-diabetic drug that can reduce the levels of insulin and insulin-like growth factor 1 in the blood that promote cell proliferation
.
In addition, it can directly activate the AMPK pathway and inhibit the proliferation of colon cancer cells [6]
.
A meta-analysis of 14 observational studies (n=459607) found that patients with type 2 diabetes who used metformin had a 27% reduction in the incidence of colorectal cancer compared with patients who did not use metformin (including those who used other treatments) (OR, 0.
73; 95% CI, 0.
62–0.
86) [7]
.
We know that the complete process of polyp carcinogenesis is "small polyps→adenoma→high-grade neoplasia→colorectal cancer"
.
So, where does metformin start its blocking effect? A meta-analysis of 5 observational studies (n=19730) found that metformin reduced the risk of adenoma in patients with type 2 diabetes by 20% (OR, 0.
80; 95% CI, 0.
71–0.
90)
.
Therefore, the blocking of the onset of colorectal cancer by metformin has already begun at least from the "polyp-adenoma" road
.
However, the editor here reminds everyone that although metformin is good, it is only suitable for the prevention of diabetic patients! It is not suitable for ordinary people who have no disease or disaster.
.
.
Except for aspirin and metformin which are recommended by AGA, the other 5 drugs are not recommended for the following reasons: 1.
Other non-aspirin NSAIDs drugs ■ AGA guidelines regulations due to non- Aspirin-like NSAIDs have a higher risk of cardiovascular and gastrointestinal adverse events.
Therefore, for people with a general risk of colorectal cancer, clinicians are not recommended to use these drugs
.
■ Recommended background.
In the past, two trials explored the effect of COX-2 inhibitors on the recurrence of adenomas [8-9].
However, due to the increased risk of cardiovascular events caused by COX-2 inhibitors, both studies were forced to terminate early
.
For non-selective non-steroidal anti-inflammatory drugs, gastrointestinal toxicity (peptic ulcer, gastrointestinal bleeding) is the main risk, and the increase in risk is related to the dose of the drug
.
2.
Calcium or Vitamin D ■ AGA Guidelines Regulations Clinicians should not use calcium or vitamin D (alone or in combination) to prevent colorectal tumors
.
■ Recommended background 1.
Calcium Calcium is an essential nutrient for the human body and has a variety of biochemical functions
.
For a long time, it has been believed that calcium can inhibit cell proliferation by binding to harmful free fatty acids and bile acids in the intestine, thereby preventing the occurrence of colorectal cancer [10]
.
Is it true? In fact, this point is full of controversy
.
Many observational studies have linked dietary intake and/or additional calcium supplementation with a reduction in the risk of colorectal cancer [11-13]
.
One of the largest studies was the 2016 analysis of nurse health studies and health professionals follow-up studies.
The study reached three key conclusions [14]: higher calcium intake and lower results The risk of rectal cancer is related (RR, 0.
78; 95% CI, 0.
65–0.
95); the relationship between calcium intake and the risk of colorectal cancer seems to be dose-dependent; dietary calcium intake and additional calcium supplementation have effects on colorectal cancer There does not seem to be a difference in the degree of reduction in morbidity
.
Based on these data, American Cancer Research even publicly stated that calcium supplements can reduce the risk of colorectal cancer [15]
.
However, the results of a recent larger randomized study suggest that calcium supplementation is not beneficial for the prevention of adenomas [16]
.
Some follow-up studies have also found that calcium supplementation is associated with an increased risk of sessile serrated polyps (RR, 2.
66; 95% CI, 1.
44–4.
89) [17]
.
More seriously, high calcium intake can increase the risk of prostate cancer [13], and excessive use of calcium supplements can also lead to nephrotoxicity, hypercalcemia and other metabolic abnormalities
.
2.
Vitamin D There is evidence that vitamin D has anti-proliferative effects in various tissues in the body (including colon).
In addition, the lack of vitamin D is also related to the occurrence of colorectal cancer
.
Most importantly, vitamin D has long been widely used as a dietary supplement worldwide and is relatively safe
.
However, many observational studies have investigated the association between vitamin D supplementation and the incidence of colorectal cancer or adenoma, and have not produced consistent results [18-26]
.
3.
Folic acid ■ AGA guidelines and regulations clinicians should not use folic acid to prevent colorectal tumors
.
■ Recommended background Folic acid (vitamin B9) is an essential nutrient that has many important functions in the body
.
There is evidence that folic acid can inhibit the occurrence of colorectal cancer through a variety of mechanisms, including maintaining DNA synthesis and repair
.
According to nurse health research and follow-up research reports of health professionals, long-term intake of large amounts of folic acid is negatively associated with the risk of colorectal cancer (RR, 0.
69; 95% CI, 0.
51-0.
94) [27]
.
However, a large multicenter trial in the United States (n=1021) found that folic acid was associated with an increased risk of advanced adenoma and multiple adenoma [28]
.
In addition, in the folic acid group, the risk of cancers other than colorectal cancer also increased, especially prostate cancer [29]
.
4.
Statins ■ AGA Guidelines Regulations For people at general risk of colorectal cancer, clinicians should not use statins to prevent colorectal tumors
.
For people with a history of colorectal cancer, clinicians should not use statins to reduce mortality
.
■ Recommended background Statins are usually widely used in the treatment of hypercholesterolemia and cardiovascular diseases
.
The drug has a variety of anti-proliferative properties and inhibits the biosynthesis of cholesterol, which plays a key role in the progression of several cancers including colorectal cancer [30]
.
The effect of statins on the chemoprevention of colorectal tumors is currently unclear
.
Therefore, statins should not be used to prevent colorectal tumors at this time
.
References: [1] International Agency for Research on Cancer.
Late stglobal cancer data: Cancer burden rises to 19.
3 million new cases and 10.
0 million cancer deaths in 2020[EB/OL].
[2021-01-10].
https://www.iarc.
fr/faq/latest-global-cancer-data-2020-qa/.
[2] Chinese Medical Association Gastroenterology Branch (CSGE), Chinese Medical Association Gastroenterology Branch Cancer Cooperation Group.
China Colorectal Cancer Prevention Consensus (2016, Shanghai).
Chinese Journal of Digestion, 2016, 36(11): 721 -733.
[3]Chubak J.
Kamineni A.
Buist DSMet al.
Aspirin use for the prevention of colorectal cancer:an updated systematic evidence review for the USPreventive Services Task Force.
USPreventive Services Task Force,Rockville,MD2015.
[4]Rothwell PMWilson M.
Elwin CEet al.
Long-term effect of aspirin on colorectal cancer incidence and mortality:20-year follow-up of five randomised trials.
Lancet.
2010;376:1741-1750.
[5]Li P.
Wu H.
Zhang H.
et al.
Aspirin use after diagnosis but not prediagnosis improves established colorectal cancer survival: a meta-analysis.
Gut.
2015;64:1419-1425.
[6]MargaretE, RichardRS.
Liver directed the rapies in metastatic colorectal cancer[J].JGastrointestinalOncol, 2014, 5(5): 374-387.
[7]Peter S.
Liang,Aasma Shaukat,Seth D.
Crockett.
AGA Clinical Practice Update on Chemoprevention for Colorectal Neoplasia:Expert Review.
Clinical Gastroenterology and Hepatology.
DOI:https://doi.
org/10.
1016/j.
cgh.
2021.
02.
014.
[8]Bresalier RSSandler RSQuan H.
et al.
Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial.
N Engl J Med.
2005;352:1092-1102.
[9]Solomon SDMcMurray JJPfeffer MAet al.
Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention.
N Engl J Med.
2005;352:1071-1080.
[10]Algire C.
Amrein L.
Zakikhani M.
et al.