-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
| 1. Sucralose worsens AOM/DSS-induced colitis-related colorectal cancer in mice, reduces body weight and colon length, increases the number/size of colorectal tumors, colitis pathology score, spleen weight and mortality;2. Trichloro Sucrose promotes the change of digestive protease activity induced by AOM/DSS, further increases the activity of trypsin and chymotrypsin, and reduces the activity of β-glucuronidase;3. Sucralose worsens the damage of intestinal barrier function induced by AOM/DSS, and Change the composition of the intestinal flora;4. Sucralose increases the expression of inflammatory factors (TNF-α, IL-1β) and TLR4/MyD88 in the colon, reduces the expression of IL-10, and up-regulates the STAT3-VEGF signal. Editor-in-Chief RecommendationSucralose is a non-calorie artificial sweetener that is used in a variety of foods and beverages. The Jiang Mingshan team of the Second Affiliated Hospital of Harbin Medical University and the Wang Xiuhong team of Harbin Medical University published a new study in Frontiers in Oncology. In a mouse model of AOM/DSS-induced colitis-related colorectal cancer, sucralose can Promote the occurrence of tumors, and cause the imbalance of intestinal flora, destroy the intestinal barrier function, reduce the activity of digestive proteases, and worsen colon inflammation. In Oncology Frontiers[the IF: 4. 848] Sucralose-Promotes the Associated Colitis in the Colorectal Cancer Risk Along With the Model A Murine Changes in Microbiota sucralose promote colitis-related risk of colorectal cancer in a mouse model, and accompanying flora 10. 3389 / fonc . 2020. 00710 2020-06-03, Article Abstract:Sucralose is a calorie-free high-intensity artificial sweetener that is widely used in thousands of foods and beverages all over the world. Although it was initially regarded as a safe, inert food additive, its adverse effect on gut microbiota and health has drawn more and more attention as evidence accumulates. Studies by us and others revealed that sucralose exacerbated gut damage and inflammation in animal models for inflammatory bowel disease (IBD), including those for both ulcerative colitis, and Crohn's disease. Our study demonstrated that sucralosetran greatly aggravated dextran sulfate sodium (DSS)-induced colitis along with causing changes in gut microbiota, the gut barrier and impaired inactivation of digestive proteases mediated by deconjugated bilirubin. It is well-documented that IBD greatly increases the risk of colorectal cancer (CRC), the globally third-most-common cancer, which, like IBD, has a high rate in the developed countries. Azoxymethane (AOM)/DSS has been the most commonly used animal model for CRC. In this study, we further explored the effect of sucralose on tumorigenesis and the possible mechanism involved using the AOM/DSS mouse model. First, 1. 5 mg/ml sucralose was included in the drinking water for 6 weeks to reach a relatively stable phase of impact on gut microbiota. Then, 10 mg/kg AOM was administered through intraperitoneal injection. Seven days later, 2. 5% DSS was put in the drinking water for 5 days, followed by 2 weeks without DSS. The 5 days of DSS was then repeated, and the mice were sacrificed 6 weeks after AOM injection. The results showed that sucralose caused significant increases in the number and size of AOM/DSS-induced colorectal tumors along with changes in other parameters such as body and spleen weight, pathological scores, mortality, fecal β-glucuronidase and digestive proteases, gut barrier molecules , gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor-associated signaling pathway molecules. These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation. fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules. These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation. fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules. These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation. damage to the gut barrier, and exacerbated inflammation. damage to the gut barrier, and exacerbated inflammation. First Authors: Xueting Li Correspondence Authors: Xiuhong Wang,Mingshan Jiang All Authors: Xueting Li,Yuanli Liu,Yan Wang,Xue Li,Xinran Liu,Mengru Guo,Yiwei Tan,Xiaofa Qin,Xiuhong Wang,Mingshan Jiang Disclaimer: This article only represents the author's personal views and has nothing to do with China Probiotics. com. The originality and the text and content stated in the article have not been verified by this site. This site does not make any guarantee or commitment to the authenticity, completeness, and timeliness of this article, all or part of the content, and the text. Please readers for reference only, and please Verify the relevant content yourself. Copyright Notice 1. Some of the reprinted articles on this site are not original, and the copyright and liability belong to the original author. 2. All reprinted articles, links and pictures on this website are for the purpose of conveying more information, and clearly indicate the source and author. Media or individuals who do not want to be reprinted can contact us for infringement information that can provide sufficient evidence , Bio149 will be deleted within 12 hours after confirmation. 3. Users are welcome to post original articles to 86371366@qq. com, and publish them to the homepage after review. The copyright and liability belong to the sender. |
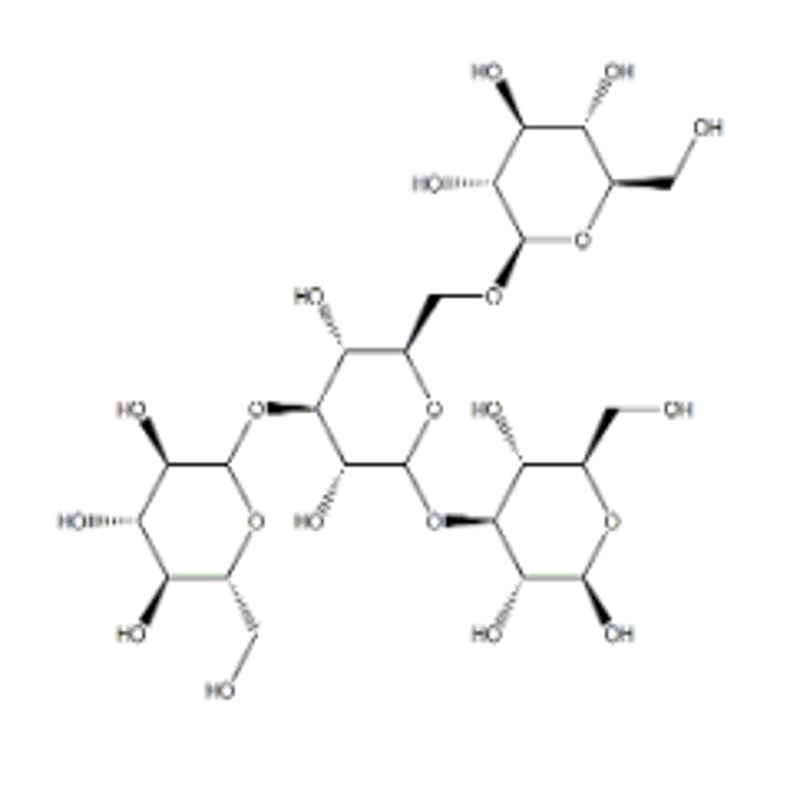
Sucralose worsens AOM/DSS-induced colitis-related colorectal cancer in mice, reduces body weight and colon length, increases the number/size of colorectal tumors, colitis pathology score, spleen weight and mortality; 2.
Trichloro Sucrose promotes the change of digestive protease activity induced by AOM/DSS, further increases the activity of trypsin and chymotrypsin, and reduces the activity of β-glucuronidase; 3.
Sucralose worsens the damage of intestinal barrier function induced by AOM/DSS, and Change the composition of the intestinal flora; 4.
Sucralose increases the expression of inflammatory factors (TNF-α, IL-1β) and TLR4/MyD88 in the colon, reduces the expression of IL-10, and up-regulates the STAT3-VEGF signal.
Editor-in-Chief Recommendation Sucralose is a non-calorie artificial sweetener that is used in a variety of foods and beverages.
The Jiang Mingshan team of the Second Affiliated Hospital of Harbin Medical University and the Wang Xiuhong team of Harbin Medical University published a new study in Frontiers in Oncology.
In a mouse model of AOM/DSS-induced colitis-related colorectal cancer, sucralose can Promote the occurrence of tumors, and cause the imbalance of intestinal flora, destroy the intestinal barrier function, reduce the activity of digestive proteases, and worsen colon inflammation.
In Oncology Frontiers [the IF: 4.
848] Sucralose-Promotes the Associated Colitis in the Colorectal Cancer Risk Along With the Model A Murine Changes in Microbiota sucralose promote colitis-related risk of colorectal cancer in a mouse model, and accompanying flora 10.
3389 / fonc .
2020.
00710
2020-06-03, Article Abstract:Sucralose is a calorie-free high-intensity artificial sweetener that is widely used in thousands of foods and beverages all over the world.
Although it was initially regarded as a safe, inert food additive, its adverse effect on gut microbiota and health has drawn more and more attention as evidence accumulates.
Studies by us and others revealed that sucralose exacerbated gut damage and inflammation in animal models for inflammatory bowel disease (IBD), including those for both ulcerative colitis, and Crohn's disease.
Our study demonstrated that sucralosetran greatly aggravated dextran sulfate sodium (DSS)-induced colitis along with causing changes in gut microbiota, the gut barrier and impaired inactivation of digestive proteases mediated by deconjugated bilirubin.
It is well-documented that IBD greatly increases the risk of colorectal cancer (CRC), the globally third-most-common cancer, which, like IBD, has a high rate in the developed countries.
Azoxymethane (AOM)/DSS has been the most commonly used animal model for CRC.
In this study, we further explored the effect of sucralose on tumorigenesis and the possible mechanism involved using the AOM/DSS mouse model.
First, 1.
5 mg/ml sucralose was included in the drinking water for 6 weeks to reach a relatively stable phase of impact on gut microbiota.
Then, 10 mg/kg AOM was administered through intraperitoneal injection.
Seven days later, 2.
5% DSS was put in the drinking water for 5 days, followed by 2 weeks without DSS.
The 5 days of DSS was then repeated, and the mice were sacrificed 6 weeks after AOM injection.
The results showed that sucralose caused significant increases in the number and size of AOM/DSS-induced colorectal tumors along with changes in other parameters such as body and spleen weight, pathological scores, mortality, fecal β-glucuronidase and digestive proteases, gut barrier molecules , gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor-associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
damage to the gut barrier, and exacerbated inflammation.
damage to the gut barrier, and exacerbated inflammation. First Authors:
Xueting Li
Correspondence Authors: Xiuhong
Wang,Mingshan Jiang
All Authors:
Xueting Li,Yuanli Liu,Yan Wang,Xue Li,Xinran Liu,Mengru Guo,Yiwei Tan,Xiaofa Qin,Xiuhong Wang,Mingshan Jiang
Disclaimer: This article only represents the author's personal views and has nothing to do with China Probiotics.
com.
The originality and the text and content stated in the article have not been verified by this site.
This site does not make any guarantee or commitment to the authenticity, completeness, and timeliness of this article, all or part of the content, and the text.
Please readers for reference only, and please Verify the relevant content yourself.
com.
The originality and the text and content stated in the article have not been verified by this site.
This site does not make any guarantee or commitment to the authenticity, completeness, and timeliness of this article, all or part of the content, and the text.
Please readers for reference only, and please Verify the relevant content yourself.
Copyright Notice
1.
Some of the reprinted articles on this site are not original, and the copyright and liability belong to the original author.
2.
All reprinted articles, links and pictures on this website are for the purpose of conveying more information, and clearly indicate the source and author.
Media or individuals who do not want to be reprinted can contact us for infringement information that can provide sufficient evidence , Bio149 will be deleted within 12 hours after confirmation.
3.
Users are welcome to post original articles to 86371366@qq.
com, and publish them to the homepage after review.
The copyright and liability belong to the sender.
1. Some of the reprinted articles on this site are not original, and the copyright and liability belong to the original author.
2.
All reprinted articles, links and pictures on this website are for the purpose of conveying more information, and clearly indicate the source and author.
Media or individuals who do not want to be reprinted can contact us for infringement information that can provide sufficient evidence , Bio149 will be deleted within 12 hours after confirmation.
3.
Users are welcome to post original articles to 86371366@qq.
com, and publish them to the homepage after review.
The copyright and liability belong to the sender.
Sucralose worsens AOM/DSS-induced colitis-related colorectal cancer in mice, reduces body weight and colon length, increases the number/size of colorectal tumors, colitis pathology score, spleen weight and mortality; 2.
Trichloro Sucrose promotes the change of digestive protease activity induced by AOM/DSS, further increases the activity of trypsin and chymotrypsin, and reduces the activity of β-glucuronidase; 3.
Sucralose worsens the damage of intestinal barrier function induced by AOM/DSS, and Change the composition of the intestinal flora; 4.
Sucralose increases the expression of inflammatory factors (TNF-α, IL-1β) and TLR4/MyD88 in the colon, reduces the expression of IL-10, and up-regulates the STAT3-VEGF signal.
Editor-in-Chief Recommendation Sucralose is a non-calorie artificial sweetener that is used in a variety of foods and beverages.
The Jiang Mingshan team of the Second Affiliated Hospital of Harbin Medical University and the Wang Xiuhong team of Harbin Medical University published a new study in Frontiers in Oncology.
In a mouse model of AOM/DSS-induced colitis-related colorectal cancer, sucralose can Promote the occurrence of tumors, and cause the imbalance of intestinal flora, destroy the intestinal barrier function, reduce the activity of digestive proteases, and worsen colon inflammation.
In Oncology Frontiers [the IF: 4.
848] Sucralose-Promotes the Associated Colitis in the Colorectal Cancer Risk Along With the Model A Murine Changes in Microbiota sucralose promote colitis-related risk of colorectal cancer in a mouse model, and accompanying flora 10.
3389 / fonc .
2020.
00710
2020-06-03, Article Abstract:Sucralose is a calorie-free high-intensity artificial sweetener that is widely used in thousands of foods and beverages all over the world.
Although it was initially regarded as a safe, inert food additive, its adverse effect on gut microbiota and health has drawn more and more attention as evidence accumulates.
Studies by us and others revealed that sucralose exacerbated gut damage and inflammation in animal models for inflammatory bowel disease (IBD), including those for both ulcerative colitis, and Crohn's disease.
Our study demonstrated that sucralosetran greatly aggravated dextran sulfate sodium (DSS)-induced colitis along with causing changes in gut microbiota, the gut barrier and impaired inactivation of digestive proteases mediated by deconjugated bilirubin.
It is well-documented that IBD greatly increases the risk of colorectal cancer (CRC), the globally third-most-common cancer, which, like IBD, has a high rate in the developed countries.
Azoxymethane (AOM)/DSS has been the most commonly used animal model for CRC.
In this study, we further explored the effect of sucralose on tumorigenesis and the possible mechanism involved using the AOM/DSS mouse model.
First, 1.
5 mg/ml sucralose was included in the drinking water for 6 weeks to reach a relatively stable phase of impact on gut microbiota.
Then, 10 mg/kg AOM was administered through intraperitoneal injection.
Seven days later, 2.
5% DSS was put in the drinking water for 5 days, followed by 2 weeks without DSS.
The 5 days of DSS was then repeated, and the mice were sacrificed 6 weeks after AOM injection.
The results showed that sucralose caused significant increases in the number and size of AOM/DSS-induced colorectal tumors along with changes in other parameters such as body and spleen weight, pathological scores, mortality, fecal β-glucuronidase and digestive proteases, gut barrier molecules , gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor-associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
damage to the gut barrier, and exacerbated inflammation.
damage to the gut barrier, and exacerbated inflammation. First Authors:
Xueting Li
Correspondence Authors: Xiuhong
Wang,Mingshan Jiang
All Authors:
Xueting Li,Yuanli Liu,Yan Wang,Xue Li,Xinran Liu,Mengru Guo,Yiwei Tan,Xiaofa Qin,Xiuhong Wang,Mingshan Jiang
Disclaimer: This article only represents the author's personal views and has nothing to do with China Probiotics.
com.
The originality and the text and content stated in the article have not been verified by this site.
This site does not make any guarantee or commitment to the authenticity, completeness, and timeliness of this article, all or part of the content, and the text.
Please readers for reference only, and please Verify the relevant content yourself.
com.
The originality and the text and content stated in the article have not been verified by this site.
This site does not make any guarantee or commitment to the authenticity, completeness, and timeliness of this article, all or part of the content, and the text.
Please readers for reference only, and please Verify the relevant content yourself.
Copyright Notice
1.
Some of the reprinted articles on this site are not original, and the copyright and liability belong to the original author.
2.
All reprinted articles, links and pictures on this website are for the purpose of conveying more information, and clearly indicate the source and author.
Media or individuals who do not want to be reprinted can contact us for infringement information that can provide sufficient evidence , Bio149 will be deleted within 12 hours after confirmation.
3.
Users are welcome to post original articles to 86371366@qq.
com, and publish them to the homepage after review.
The copyright and liability belong to the sender.
1. Some of the reprinted articles on this site are not original, and the copyright and liability belong to the original author.
2.
All reprinted articles, links and pictures on this website are for the purpose of conveying more information, and clearly indicate the source and author.
Media or individuals who do not want to be reprinted can contact us for infringement information that can provide sufficient evidence , Bio149 will be deleted within 12 hours after confirmation.
3.
Users are welcome to post original articles to 86371366@qq.
com, and publish them to the homepage after review.
The copyright and liability belong to the sender.
Sucralose worsens AOM/DSS-induced colitis-related colorectal cancer in mice, reduces body weight and colon length, increases the number/size of colorectal tumors, colitis pathology score, spleen weight and mortality; 2.
Trichloro Sucrose promotes the change of digestive protease activity induced by AOM/DSS, further increases the activity of trypsin and chymotrypsin, and reduces the activity of β-glucuronidase; 3.
Sucralose worsens the damage of intestinal barrier function induced by AOM/DSS, and Change the composition of the intestinal flora; 4.
Sucralose increases the expression of inflammatory factors (TNF-α, IL-1β) and TLR4/MyD88 in the colon, reduces the expression of IL-10, and up-regulates the STAT3-VEGF signal.
Editor-in-Chief Recommendation Sucralose is a non-calorie artificial sweetener that is used in a variety of foods and beverages.
The Jiang Mingshan team of the Second Affiliated Hospital of Harbin Medical University and the Wang Xiuhong team of Harbin Medical University published a new study in Frontiers in Oncology.
In a mouse model of AOM/DSS-induced colitis-related colorectal cancer, sucralose can Promote the occurrence of tumors, and cause the imbalance of intestinal flora, destroy the intestinal barrier function, reduce the activity of digestive proteases, and worsen colon inflammation.
In Oncology Frontiers
[the IF: 4.
848] Sucralose-Promotes the Associated Colitis in the Colorectal Cancer Risk Along With the Model A Murine Changes in Microbiota sucralose promote colitis-related risk of colorectal cancer in a mouse model, and accompanying flora 10.
3389 / fonc .
2020.
00710
2020-06-03, Article Abstract:Sucralose is a calorie-free high-intensity artificial sweetener that is widely used in thousands of foods and beverages all over the world.
Although it was initially regarded as a safe, inert food additive, its adverse effect on gut microbiota and health has drawn more and more attention as evidence accumulates.
Studies by us and others revealed that sucralose exacerbated gut damage and inflammation in animal models for inflammatory bowel disease (IBD), including those for both ulcerative colitis, and Crohn's disease.
Our study demonstrated that sucralosetran greatly aggravated dextran sulfate sodium (DSS)-induced colitis along with causing changes in gut microbiota, the gut barrier and impaired inactivation of digestive proteases mediated by deconjugated bilirubin.
It is well-documented that IBD greatly increases the risk of colorectal cancer (CRC), the globally third-most-common cancer, which, like IBD, has a high rate in the developed countries.
Azoxymethane (AOM)/DSS has been the most commonly used animal model for CRC.
In this study, we further explored the effect of sucralose on tumorigenesis and the possible mechanism involved using the AOM/DSS mouse model.
First, 1.
5 mg/ml sucralose was included in the drinking water for 6 weeks to reach a relatively stable phase of impact on gut microbiota.
Then, 10 mg/kg AOM was administered through intraperitoneal injection.
Seven days later, 2.
5% DSS was put in the drinking water for 5 days, followed by 2 weeks without DSS.
The 5 days of DSS was then repeated, and the mice were sacrificed 6 weeks after AOM injection.
The results showed that sucralose caused significant increases in the number and size of AOM/DSS-induced colorectal tumors along with changes in other parameters such as body and spleen weight, pathological scores, mortality, fecal β-glucuronidase and digestive proteases, gut barrier molecules , gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor-associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
fecal β-glucuronidase and digestive proteases, gut barrier molecules, gut microbiota, inflammatory cytokines and pathways (TNFα, IL-1β, IL-6, IL-10, and TLR4/Myd88/NF-κB signaling), and STAT3/VEGF tumor -associated signaling pathway molecules.
These results suggest that sucralose may increase tumorigenesis along with dysbiosis of gut microbiota, impaired inactivation of digestive protease, damage to the gut barrier, and exacerbated inflammation.
damage to the gut barrier, and exacerbated inflammation.
damage to the gut barrier, and exacerbated inflammation. First Authors:
Xueting Li
Correspondence Authors: Xiuhong
Wang,Mingshan Jiang
All Authors:
Xueting Li,Yuanli Liu,Yan Wang,Xue Li,Xinran Liu,Mengru Guo,Yiwei Tan,Xiaofa Qin,Xiuhong Wang,Mingshan Jiang