-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*It is only for medical professionals to read and refer to classic cases, worthy of collection! Case review: The patient was a 59-year-old man, a farmer, and was admitted to the hospital for 1 day due to dizziness.
▎History of present illness: 1 day ago, the patient developed dizziness without obvious inducement, which was rotating, accompanied by nausea and vomiting, which worsened after exercise, and pain around the right ear.
There was no obvious abnormality in brain CT in our hospital.
He was given "sedation and analgesia" The effect of other drug treatments was average, dizziness worsened, unable to stand, nausea and vomiting were obvious, and he was admitted to the hospital with "dizziness pending investigation".
▎Past history: surgery for "appendicitis" was performed 3 months ago, and the postoperative recovery is good; deny the history of hypertension, diabetes, coronary heart disease; long-term history of heavy smoking; deny the history of taking special drugs; deny the history of pre-infection and vaccination .
▎Admission examination: T 36.
4℃, P 51 beats/min, R 18 beats/min, BP 129/86mmHg.
Consciousness, clear articulation, bilateral pupils with equal circles, diameter 0.
3cm, bilateral pupils reflect light (+), visible horizontal leftward rapid nystagmus, bilateral nasolabial folds symmetrical, mouth angles symmetrical, tongue sticking out in the middle , Pharyngeal reflex is normal, neck is soft, limb muscle tone is normal, limb muscle strength is grade 5, sensation is normal, bilateral tendon reflex (++), bilateral Pap's sign is negative, both lungs are clear, no dryness is heard Rales, regular heart rhythm, no murmur, soft abdomen, no tenderness, rebound pain, no edema of both lower limbs.
▎Complete relevant auxiliary examinations on the same day: CT of the brain showed no obvious abnormalities in the brain parenchyma, and the right maxillary sinus cyst.
The ECG shows sinus rhythm and sinus bradycardia.
Consider the diagnosis? Preliminary consideration of peripheral dizziness, aspirin enteric-coated tablets to prevent platelet aggregation, atorvastatin to stabilize plaques, betahistine mesylate, gastrodin to stop dizziness, Shuxuening to improve microcirculation and other treatments.
The patient's condition progressed on the second day of admission: the patient developed a skewed mouth, peripheral facial paralysis on the right side, slurred speech, dizziness and nystagmus, and the remaining symptoms were the same as admitted to the hospital.
▎Physical examination: dysarthria, shallow forehead lines on the right side, poor eyesight closed on the right side, 4mm whiteness, shallow nasolabial fold on the right side, low angle of mouth on the right side, middle tongue extension, tendon reflexes of the limbs (+), remaining physical examination Same admission.
▎Blood test results: blood routine, erythrocyte sedimentation rate, liver and kidney function, blood lipids, rheumatism, thyroid function, glycosylated hemoglobin, electrolytes, and viruses are roughly normal.
▎Vascular ultrasound: Intima-media thickening with plaque formation at the left carotid bifurcation.
Cardiac ultrasound: aortic regurgitation (small amount), tricuspid regurgitation (small amount).
Head MRI showed that: 1.
No obvious abnormalities were found on plain MRI; 2.
Right maxillary sinus mucosal cyst; 3.
Right internal carotid artery A1 segment mild stenosis; 4.
Right middle anterior cerebral artery bifurcation Suspected aneurysm; 5.
Enlargement of the right ocular artery.
Location diagnosis? Qualitative diagnosis? Positioning: According to the patient's dizziness and nystagmus, considering the vestibular nerve damage, according to the right peripheral facial paralysis, considering the facial nerve damage.
Qualitative: The patient had no abnormalities in head MRI, except for cerebrovascular disease.
Combined with peripheral facial paralysis on the right side of the patient, there was pain around the right ear when dizziness occurred.
Consider viral infection? The diagnosis of the disease considers the possibility of Bell's palsy, while brainstem encephalitis cannot be excluded.
Adjust the treatment plan: add acyclovir to fight infection.
On the third day, the patient's condition continued to progress: the patient developed bilateral peripheral facial paralysis, general fatigue, and the remaining symptoms were the same as before.
Physical examination: Bilateral closed eyes difference, 4mm whiteness, bilateral frontal lines symmetrical, bilateral nasolabial folds symmetrical, mouth angle symmetrical, tongue extension centered, bilateral knee reflex, Achilles tendon reflex (-), upper limb tendon reflex (+ ), the same as before.
The diagnosis was further improved.
Lumbar puncture showed that the cerebrospinal fluid was colorless and clear, and the pressure was 175mmH20.
White blood cells 10×10-6/L, cerebrospinal fluid protein 1745.
1 mg/L↑, cerebrospinal fluid lactate dehydrogenase 28.
00 U/L↑.
Cerebrospinal fluid immunoglobulin G 280.
00 mg/L↑, cerebrospinal fluid immunoglobulin A 38.
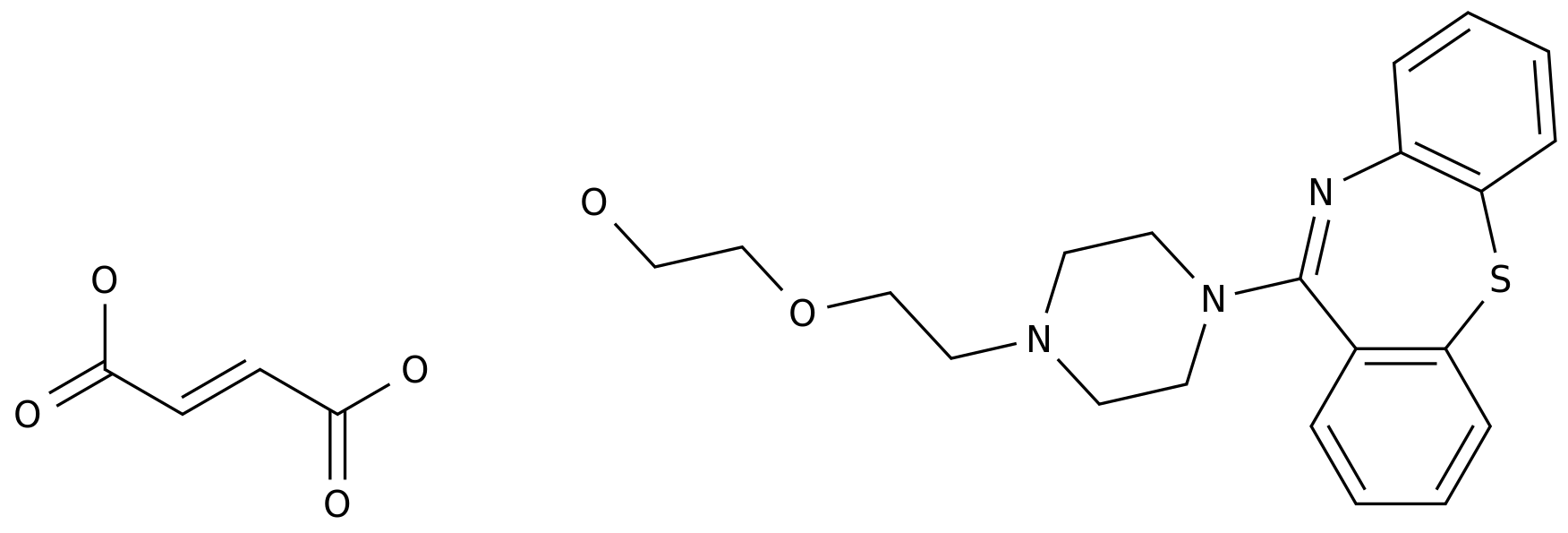
40 mg/L↑, sugar and chloride were normal. Serum peripheral neuropathy series antibodies showed positive anti-Sulfatide antibody IgG class.
The electromyography of the extremities showed the manifestation of peripheral neurogenic damage, and there was no obvious increase or decrease in repetitive electrical stimulation.
(The picture above shows the results of a series of antibodies against serum autoimmune peripheral neuropathy) Confirm the diagnosis: Guillain-Barré syndrome (Guillain-Barrésyndrome, GBS).
He was treated with immunoglobulin and neurotrophic drugs, and was discharged from hospital after dizziness, nystagmus, and bilateral paralysis improved.
Discussion For GBS with dizziness onset, there are also a small number of reports in the previous literature, which may be related to the involvement of the cerebellar efferent pathway in the brainstem and/or the vestibular nucleus.
The patient developed bilateral peripheral facial paralysis soon after the onset of dizziness, weakened tendon reflexes, separated cerebrospinal fluid protein cells, and positive serum peripheral neuropathy series antibodies, all supporting GBS.
The subtype diagnosis considers acute inflammatory demyelination.
Hair nerve root neuropathy (AIDP).
AIDP is also the most common subtype of GBS.
The main pathology is segmental demyelination of multiple nerve roots and peripheral nerves.
Studies have shown that 45%-75% of GBS patients are found to have cranial nerve involvement.
Among them, bilateral facial nerve palsy is the most common.
Common, followed by glossopharyngeal and vagus nerves.
Some patients may have cranial nerve damage as the first symptom.
Bilateral nerve palsy is rare in clinical practice, accounting for 0.
3% to 2% of all facial nerve palsy.
Bilateral nerve palsy may occur simultaneously or alternately on both sides.
Studies have shown that the causes of facial nerve palsy can include trauma, infection, systemic, autoimmune, idiopathic, toxic, iatrogenic, tumor, metabolic, genetic and other causes.
With the help of literature, we summarize the causes of bifacial nerve palsy as follows: In summary, there are many causes of bifacial nerve palsy.
Guillain-Barré syndrome, which is manifested by bifacial paralysis, needs to be common with Bell's palsy and neuro-Lyme disease.
Identification of the reasons. Summary and perception: GBS has many forms, some of which can be dizzy and onset of bilateral paralysis.
When one lateral nerve palsy occurs, it is easy to be misdiagnosed as facial neuritis in the early stage.
For such patients, attention should be paid to the accompanying symptoms and changes in tendon reflexes.
As the condition evolves, diagnose as soon as possible to avoid delays in the diagnosis and treatment of patients due to missed diagnosis and misdiagnosis.
Reference materials: [1]Junyang,Jung,Dong Choon,Park,Su Young,Jung,Myung Jin,Park,Sang Hoon,Kim,Seung Geun,Yeo.
Bilateral facial palsy.
[J].
Acta oto-laryngologica,2019, 139(10):934-938.
[2] Chinese Medical Association Neurology Branch, Chinese Medical Association Neurology Branch Peripheral Neuropathy Cooperative Group, Chinese Medical Association Neurology Branch Electromyography and Clinical Neuroelectrophysiology Group, Chinese Medical Association Neuropathy Neuromuscular Disease Group of the Academic Branch.
Guidelines for Diagnosis and Treatment of Guillain-Barré Syndrome in China 2019[J].
Chinese Journal of Neurology,2019,52(11):877-882.
[3]Price T,Fife DG.
Bilateral simultaneous facial nerve palsy.
[J].
The Journal of laryngology and otology.
,2002,116(1):46-48.
[4]Yu Bo,Hu Kun,Yang Xiao,Chen Guisheng.
8 cases of variant Jilan-Barre Syndrome clinical analysis[J].
Journal of Ningxia Medical University,2018,40(6):712-714.
▎History of present illness: 1 day ago, the patient developed dizziness without obvious inducement, which was rotating, accompanied by nausea and vomiting, which worsened after exercise, and pain around the right ear.
There was no obvious abnormality in brain CT in our hospital.
He was given "sedation and analgesia" The effect of other drug treatments was average, dizziness worsened, unable to stand, nausea and vomiting were obvious, and he was admitted to the hospital with "dizziness pending investigation".
▎Past history: surgery for "appendicitis" was performed 3 months ago, and the postoperative recovery is good; deny the history of hypertension, diabetes, coronary heart disease; long-term history of heavy smoking; deny the history of taking special drugs; deny the history of pre-infection and vaccination .
▎Admission examination: T 36.
4℃, P 51 beats/min, R 18 beats/min, BP 129/86mmHg.
Consciousness, clear articulation, bilateral pupils with equal circles, diameter 0.
3cm, bilateral pupils reflect light (+), visible horizontal leftward rapid nystagmus, bilateral nasolabial folds symmetrical, mouth angles symmetrical, tongue sticking out in the middle , Pharyngeal reflex is normal, neck is soft, limb muscle tone is normal, limb muscle strength is grade 5, sensation is normal, bilateral tendon reflex (++), bilateral Pap's sign is negative, both lungs are clear, no dryness is heard Rales, regular heart rhythm, no murmur, soft abdomen, no tenderness, rebound pain, no edema of both lower limbs.
▎Complete relevant auxiliary examinations on the same day: CT of the brain showed no obvious abnormalities in the brain parenchyma, and the right maxillary sinus cyst.
The ECG shows sinus rhythm and sinus bradycardia.
Consider the diagnosis? Preliminary consideration of peripheral dizziness, aspirin enteric-coated tablets to prevent platelet aggregation, atorvastatin to stabilize plaques, betahistine mesylate, gastrodin to stop dizziness, Shuxuening to improve microcirculation and other treatments.
The patient's condition progressed on the second day of admission: the patient developed a skewed mouth, peripheral facial paralysis on the right side, slurred speech, dizziness and nystagmus, and the remaining symptoms were the same as admitted to the hospital.
▎Physical examination: dysarthria, shallow forehead lines on the right side, poor eyesight closed on the right side, 4mm whiteness, shallow nasolabial fold on the right side, low angle of mouth on the right side, middle tongue extension, tendon reflexes of the limbs (+), remaining physical examination Same admission.
▎Blood test results: blood routine, erythrocyte sedimentation rate, liver and kidney function, blood lipids, rheumatism, thyroid function, glycosylated hemoglobin, electrolytes, and viruses are roughly normal.
▎Vascular ultrasound: Intima-media thickening with plaque formation at the left carotid bifurcation.
Cardiac ultrasound: aortic regurgitation (small amount), tricuspid regurgitation (small amount).
Head MRI showed that: 1.
No obvious abnormalities were found on plain MRI; 2.
Right maxillary sinus mucosal cyst; 3.
Right internal carotid artery A1 segment mild stenosis; 4.
Right middle anterior cerebral artery bifurcation Suspected aneurysm; 5.
Enlargement of the right ocular artery.
Location diagnosis? Qualitative diagnosis? Positioning: According to the patient's dizziness and nystagmus, considering the vestibular nerve damage, according to the right peripheral facial paralysis, considering the facial nerve damage.
Qualitative: The patient had no abnormalities in head MRI, except for cerebrovascular disease.
Combined with peripheral facial paralysis on the right side of the patient, there was pain around the right ear when dizziness occurred.
Consider viral infection? The diagnosis of the disease considers the possibility of Bell's palsy, while brainstem encephalitis cannot be excluded.
Adjust the treatment plan: add acyclovir to fight infection.
On the third day, the patient's condition continued to progress: the patient developed bilateral peripheral facial paralysis, general fatigue, and the remaining symptoms were the same as before.
Physical examination: Bilateral closed eyes difference, 4mm whiteness, bilateral frontal lines symmetrical, bilateral nasolabial folds symmetrical, mouth angle symmetrical, tongue extension centered, bilateral knee reflex, Achilles tendon reflex (-), upper limb tendon reflex (+ ), the same as before.
The diagnosis was further improved.
Lumbar puncture showed that the cerebrospinal fluid was colorless and clear, and the pressure was 175mmH20.
White blood cells 10×10-6/L, cerebrospinal fluid protein 1745.
1 mg/L↑, cerebrospinal fluid lactate dehydrogenase 28.
00 U/L↑.
Cerebrospinal fluid immunoglobulin G 280.
00 mg/L↑, cerebrospinal fluid immunoglobulin A 38.
40 mg/L↑, sugar and chloride were normal. Serum peripheral neuropathy series antibodies showed positive anti-Sulfatide antibody IgG class.
The electromyography of the extremities showed the manifestation of peripheral neurogenic damage, and there was no obvious increase or decrease in repetitive electrical stimulation.
(The picture above shows the results of a series of antibodies against serum autoimmune peripheral neuropathy) Confirm the diagnosis: Guillain-Barré syndrome (Guillain-Barrésyndrome, GBS).
He was treated with immunoglobulin and neurotrophic drugs, and was discharged from hospital after dizziness, nystagmus, and bilateral paralysis improved.
Discussion For GBS with dizziness onset, there are also a small number of reports in the previous literature, which may be related to the involvement of the cerebellar efferent pathway in the brainstem and/or the vestibular nucleus.
The patient developed bilateral peripheral facial paralysis soon after the onset of dizziness, weakened tendon reflexes, separated cerebrospinal fluid protein cells, and positive serum peripheral neuropathy series antibodies, all supporting GBS.
The subtype diagnosis considers acute inflammatory demyelination.
Hair nerve root neuropathy (AIDP).
AIDP is also the most common subtype of GBS.
The main pathology is segmental demyelination of multiple nerve roots and peripheral nerves.
Studies have shown that 45%-75% of GBS patients are found to have cranial nerve involvement.
Among them, bilateral facial nerve palsy is the most common.
Common, followed by glossopharyngeal and vagus nerves.
Some patients may have cranial nerve damage as the first symptom.
Bilateral nerve palsy is rare in clinical practice, accounting for 0.
3% to 2% of all facial nerve palsy.
Bilateral nerve palsy may occur simultaneously or alternately on both sides.
Studies have shown that the causes of facial nerve palsy can include trauma, infection, systemic, autoimmune, idiopathic, toxic, iatrogenic, tumor, metabolic, genetic and other causes.
With the help of literature, we summarize the causes of bifacial nerve palsy as follows: In summary, there are many causes of bifacial nerve palsy.
Guillain-Barré syndrome, which is manifested by bifacial paralysis, needs to be common with Bell's palsy and neuro-Lyme disease.
Identification of the reasons. Summary and perception: GBS has many forms, some of which can be dizzy and onset of bilateral paralysis.
When one lateral nerve palsy occurs, it is easy to be misdiagnosed as facial neuritis in the early stage.
For such patients, attention should be paid to the accompanying symptoms and changes in tendon reflexes.
As the condition evolves, diagnose as soon as possible to avoid delays in the diagnosis and treatment of patients due to missed diagnosis and misdiagnosis.
Reference materials: [1]Junyang,Jung,Dong Choon,Park,Su Young,Jung,Myung Jin,Park,Sang Hoon,Kim,Seung Geun,Yeo.
Bilateral facial palsy.
[J].
Acta oto-laryngologica,2019, 139(10):934-938.
[2] Chinese Medical Association Neurology Branch, Chinese Medical Association Neurology Branch Peripheral Neuropathy Cooperative Group, Chinese Medical Association Neurology Branch Electromyography and Clinical Neuroelectrophysiology Group, Chinese Medical Association Neuropathy Neuromuscular Disease Group of the Academic Branch.
Guidelines for Diagnosis and Treatment of Guillain-Barré Syndrome in China 2019[J].
Chinese Journal of Neurology,2019,52(11):877-882.
[3]Price T,Fife DG.
Bilateral simultaneous facial nerve palsy.
[J].
The Journal of laryngology and otology.
,2002,116(1):46-48.
[4]Yu Bo,Hu Kun,Yang Xiao,Chen Guisheng.
8 cases of variant Jilan-Barre Syndrome clinical analysis[J].
Journal of Ningxia Medical University,2018,40(6):712-714.