-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
▎WuXi AppTec content team editor
.
In particular, nearly 300 million people in China suffer from liver disease, mainly including chronic hepatitis B virus (HBV) and hepatitis C virus (HCV) infections, alcoholic liver disease (ALD), non-alcoholic fatty liver disease (NAFLD) and other liver diseases
.
According to data, there are 7 million patients with cirrhosis in China, accounting for 11% of the world's deaths, of which about 78% of patients with cirrhosis are accompanied by thrombocytopenia
of varying degrees.
It can be said that thrombocytopenia is a common complication in patients with chronic liver disease and has a higher
incidence in patients with cirrhosis.
The severity of thrombocytopenia is related
to the severity of liver disease and long-term prognosis.
More importantly, severe thrombocytopenia (<50×10<b20>9/L) is a predictor of perioperative haemorrhage or rebleeding, which poses significant challenges
to surgical management.
Recently, there is increasing clinical evidence that oral small molecule thrombopoietin receptor agonists (TPO-RAs) improve thrombocytopenia
.
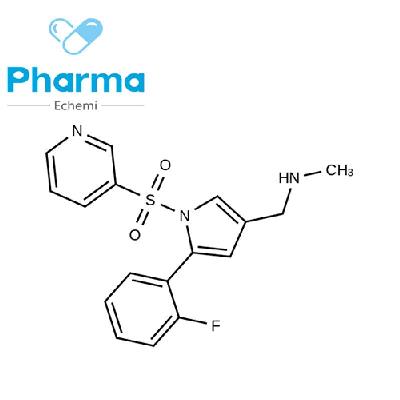
Lusutrombopag is a novel second-generation oral TPO-RAs that can act on the thrombopoietin (TPO) receptor expressed in megakaryocytes, activate the differentiation and proliferation of megakaryocytes, and promote platelet production
.
The drug has obtained marketing authorization in Japan in September 2015, the United States in August 2018, and Europe in February 2019 for the treatment of chronic liver disease with thrombocytopenia; Its application for listing registration in Chinese mainland has been accepted
.
Recently, the results of a phase 3 study of ruttrombopag in Chinese groups were officially published in Hepatology International (IF=9.
029).
This study evaluated the efficacy and safety
of rutromupag in Chinese patients with chronic liver disease with thrombocytopenia undergoing elective invasive surgery.
Results showed that ruttrombopag was effective in increasing platelet count (PLT) levels before elective invasive surgery in patients with chronic liver disease and thrombocytopenia, reducing the need for platelet transfusion, and showed a safety
profile comparable to placebo.
Professor Zhou Jian of Zhongshan Hospital affiliated to Fudan University is the corresponding author
of the study.
Screenshot credit: Hepatology International
This randomized, multicenter, placebo-controlled, double-blind, phase 3 study enrolled a total of 66 patients with chronic liver disease and severe thrombocytopenia in 9 centers in China from July 2020 to June 2021, and randomized them to rutromupag (n=44) or placebo (n=22) in a 2:1 ratio and treated with 3 mg of ruttrombopag or placebo once daily for 7 days
.
Of these, 2 patients in the placebo group missed 1 or 3 days of dosing
due to study discontinuation or drug loss.
The primary efficacy endpoint was the proportion of day 8 responders (defined as: PLT≥50×10 9/L, an increase of ≥20×109/L from baseline and no bleeding rescue therapy); The key secondary efficacy endpoint was the proportion of patients with a PLT ≥ of 50×109/L on day 8 or later and within 2 days before aggressive surgery (i.
e.
, criteria for not requiring preoperative platelet transfusion); and recorded adverse events (AEs).
The results show:
- Primary efficacy endpoint
The proportion of respondents in the ruttrombopag group was significantly higher than in the placebo group, and the difference between the two groups was statistically significant (43.
2% [19/44] vs.
4.
5% [1/22], P=0.
0011).
The median PLT values on day 8 in the rutrugopag group and placebo group were 61.
5×10 9/L and 41.
0×109/L, respectively.
The proportion of patients with PLT ≥ 50×109/L on day 8 was 68.
2% and 13.
6%, respectively.
The proportion of patients with a 2≥0×109/L increase in PLT at day 8 was 43.
2% and 4.
5%,
respectively.
▲ In the population with the full analysis set, the proportion of responders on day 8 in the rutromopaga group and the placebo group (screenshot source: Reference [1]).
- Secondary efficacy endpoints
The proportion of patients with PLTs ≥ 50×109/L on day 8 and after and 2 days before surgery was 72.
7% (32/44) in the rutrobopaar group and 18.
2% (4/22) in the placebo group, and the difference in proportion between the two groups was statistically significant (P<0.
0001).
The median maximum PLT values of the two groups were 80.
5×10 9/L and 60.
0×10 9/L, respectively.
The maximum median increase in PLT from baseline was 42.
0×10 9/L and 24.
0×109/L
, respectively.
In addition, the increase in PLT in the ruttrompag group occurred before aggressive surgery, while the increase in PLT in the placebo group occurred after aggressive surgery; The median time to reach maximum PLT in the ruttrombopag and placebo groups was 14.
5 and 27.
0 days
, respectively.
Median PLT returned to baseline within 35 days
.
▲ Change of median PLT value over time in ruttrombopag group and placebo group (screenshot source: Reference [1]).
- security
In the rutromupag group, no patients died or discontinued due to adverse events
.
Only 1 patient in the placebo group discontinued the drug
due to an adverse event.
The overall incidence of adverse events (TEAEs) during treatment was 84.
1% (37/44) in the rutromupag group and 90.
9% (20/22)
in the placebo group.
Most TEAEs have mild or moderate severity
.
The incidence of TEAE after invasive surgery is higher than before
surgery.
Drug-related adverse events
occurred in 11.
4% of patients in the rutromopag and placebo groups, respectively.
All patients had mild or moderate severity, and the incidence of drug-related AEs was less than 5%.
Three patients in the ruttrombopag group developed SAEs (hepatic encephalopathy and coagulopathy, fever, acute cholecystitis), but these were non-fatal and were not evaluated as being
related to the study drug.
During the study period, few patients reported bleeding and thrombosis-related AEs
.
Compared with placebo, the incidence of bleeding events was lower in the ruttrombopag group (6.
8% vs.
13.
6%), and only one patient developed thrombosis-associated AE (brachiocephalic vein thrombosis) of mild severity, which was assessed as unrelated
to the study drug.
Overall, the incidence of adverse events during treatment was comparable between the ruttramopag and placebo groups; Compared with overseas studies, rutromupag (3 mg) found no additional safety issues
in the Chinese patient population.
In summary, for patients with chronic liver disease and thrombocytopenia who are scheduled to receive aggressive therapy, taking 3 mg of rutromopag once daily for 7 days can effectively increase PLT to meet the criteria for aggressive surgery, thereby avoiding preoperative platelet transfusion without adding additional safety concerns
.
Crucially, in the face of tight platelet supplies, ruttrombopag is a safe, effective and reliable way to raise platelet counts before invasive surgery, providing more treatment options
for patients with chronic liver disease in China.