-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Inflammatory bowel disease (IBD), including Crohn's disease (CD) and ulcerative colitis (UC), is a chronic, recurrent, systemic, immune-mediated inflammatory disease (IMID) that can cause gastrointestinal damage
.
Current treatment regimens rely primarily on traditional drugs such as glucocorticoids, azathioprine, or biologic agents
.
However, some patients with UC and CD will lose response to current treatment regimens, so new targeted therapies
that provide sustained remission and mucosal healing are needed.
A better understanding of the pathogenesis of the disease, particularly the role of cytokines in the inflammatory cascade, has expanded the available therapeutic options
for IBD.
Monoclonal antibodies that target single cytokines, such as tumor necrosis factor-α drugs, have been approved for the treatment of IBD
.
However, a significant proportion of patients treated with monoclonal antibodies do not respond or lose their response
over time.
In addition, monoclonal antibodies require parenteral administration and may cause adverse effects, including immunogenicity
.
The intracellular JAK-STAT pathway transduces downstream signals of a variety of cytokines involved in the inflammatory cascade of IBD; Thus, targeting the JAK-STAT pathway can block multiple cytokine signals
by inhibiting a common signal transduction pathway.
Multiple JAK inhibitors have been evaluated in patients with IBD, but have produced conflicting efficacy results and have led to increased
drug toxicity due to lack of selectivity at therapeutic doses.
Based on concerns about the long-term safety of pan-JAK inhibitors, including infection (especially herpes zoster virus reactivation) and abnormalities in some human surveillance indicators, selective oral JAK inhibitors, such as Tyk2 inhibitors
, are being developed for the treatment of IBD.
JAK-STAT and TYK2 signaling pathways in IBD
The JAK family consists of 4 TYKs with different specificity, expression levels and functions, including JAK1, JAK2, JAK3 and TYK2
.
JAK1 and JAK2 mediate signal transduction via γ chains, JAK3 mediates signal transduction via 6 common γ-chain cytokines, including IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21, while TYK2 plays a key role
in mediating immune signaling via IL-10, IL-12, IL-22, IL-23, and IFNs type I and III.
The JAK-STAT pathway plays a major role
in intracellular cytokine signaling in IMID such as IBD, psoriasis (PsO), psoriatic arthritis (PsA) and lupus.
As shown in the figure below, JAK/TYK2 signaling is involved in innate immunity, acquired immunity and hematopoiesis, and is involved in cellular processes
such as cell growth, survival, differentiation and migration.
TYK2 and JAK2 regulate signal transduction pathways
downstream of IL-12 and IL-23 receptors through heterodimerization.
In addition, IL-12 is involved in the development of Th1 cells and the production of pro-inflammatory cytokine tumor necrosis factor-α and IFN-γ, while IL-23 mediates the expansion and survival of Th17 cells; Th1 and Th17 cells synergistically amplify inflammatory effects
.
In addition, TYK2 with JAK1 heterodimerization regulates the signal transduction pathways IFN-α and IFN-β downstream of the type I IFN receptor, which are involved in various functions of the immune system, including regulation of dendritic cell maturation and activation, expression of major histocompatibility complex and co-stimulatory molecules, regulation of B cell differentiation and antibody production, and regulation
of T cell survival.
TYK2-mediated IL-12, IL-23, and type I IFN signaling activates STAT-dependent transcriptional and functional responses to perpetuate
chronic inflammation.
The role of TYK2 signaling pathway inhibition in IBD
Currently, multiple clinical trials are evaluating the therapeutic strategy
of TYK2 inhibition in the treatment of IMIDS, including IBD, PsO, PsA, and lupus.
TYK2 mutations result in almost complete loss of function and impaired signaling of IL-12, IL-23, and type I IFN, but are not associated with
immunodeficiency or increased risk of infection or malignancy.
Three TYK2 inhibitors are in clinical development or are recently in clinical development for moderate to severe IBD:
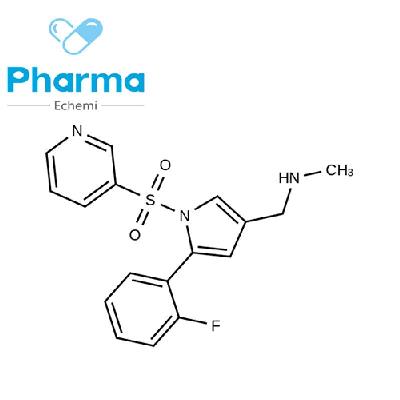
Brepocitinib
Brepocitinib, a dual oral TYK2/JAK1 inhibitor that binds to active sites in the TYK2 and JAK1 catalytic domains, is currently evaluating the efficacy and safety
of brepocitinib in PsO, PsA, IBD (UC and CD) and lupus 。 In a Phase 2a clinical trial in patients with moderate to severe plaque PsO, brepocitinib 30 mg once daily, 60 mg once daily, or placebo were received during the 4-week induction period, followed by brepocitinib 10 mg once daily and 30 mg once daily to evaluate their efficacy and safety
。 The results showed that the change in psoriasis area and severity index (PASI) from baseline (primary endpoint) at week 12 was significantly higher in patients with oral brepocitinib than in the placebo group (P < 0.
05).
Patients who were still receiving 30 mg once daily up to week 12 had the highest
response rate to PASI-75 compared to the placebo group.
Currently, two trials are evaluating the efficacy and safety
of oral brepocitinib in patients with moderate to severe UC or CD.
Trials on active PsA will be completed in 2021, while trials on lupus are
ongoing.
PF-06826647
PF-06826647 is a dual oral TYK2/JAK2 inhibitor that binds
to active sites in the TYK2 and JAK2 catalytic domains.
In human whole blood tests, PF-06826647 binding to TYK2 can strongly inhibit IL-12 and IL-23 signal transduction
.
In a phase I study of patients with moderate to severe plaque PsO, PF-06826647 400 mg once daily resulted in a significant improvement
in PASI scores relative to baseline at 4 weeks of treatment.
PF-06826647 The severity of adverse events in all treatments in patients treated was mild
.
At week 4, significant reductions
in IL-17A and IL-17F expression were observed in the PF-06826647 group.
A phase II trial evaluating the efficacy and safety of PF-06826647 in patients with moderate to severe PsO was completed in 2020 (ClinicalTrials.
gov identification number: gov identifier: NCT03895372).
In a UC trial that planned to compare 4 doses of PF-06826647 with placebo during an 8-week double-blind induction period followed by a 52-week open-label extension period, the primary endpoints were endoscopic response at week 8 and long-term safety at week 60, with an estimated completion date of October 2023; However, the study was withdrawn
.
Deucravacitinib
Deucravacitinib (formerly BMS-986165) is a novel, oral, selective TYK2 inhibitor with a different
mechanism of action than JAK1-3 inhibitors.
Deucravacitinib inhibits TYK2 by binding to the regulatory (JH2
pseudokinase) domain rather than directly to the active site in the catalytic domain like JAK1-3 inhibitors.
。 Locking the regulatory domain to an inhibitory interaction with the catalytic domain by allosteric binding inactivates TYK2, thereby preventing receptor-mediated activation and downstream signal transduction
.
Deucravacitinib is a highly selective TYK2 inhibitor with very low or no activity against JAK1-3 (in contrast, JAK1-3 inhibitors do not bind to the regulatory domain of TYK2).
In cell-based experiments, deucravacitinib was more than 100 times more selective for JAK1/JAK3 and more than 2000 times as selective for JAK2 (half of the maximum inhibitory concentration [IC50] data).
Deucravacitinib's selectivity for TYK2 reduces the likelihood of toxicity, such as that associated with JAK1-3 inhibitors
.
In addition, deucravacitinib treatment of human peripheral blood mononuclear cells inhibits the production of γ-induced proteins stimulated by IFN-α with an IC50 of 6 nM, confirming that deucravacitinib inhibits TYK2-dependent functional cell effects
mediated by IFN stimulation.
In addition, deucravacitinib dose-dependently inhibits IL-23-mediated STAT3 phosphorylation
in CD161+CD3+TH17 cells in human peripheral blood mononuclear cells.
Disruption of IL-23 signaling leads to inhibition of CD4+ T cell production of IL-17 with an IC50 of 2 nM
.
Oral deucravacitinib is currently being evaluated as a treatment option for several IMIDs: PsO, PsA, IBD (UC and CD), and lupus (including lupus nephritis).
Summary
Treatment of IBD requires new oral therapies
that are safe and effective.
JAK1-3 inhibitors have been shown to be inconsistent in efficacy for IBD and associated with
toxicity.
In addition, TYK2 plays a central role
in the pathophysiology of IBD by regulating signal transduction and functional response downstream of IL-12, IL-23, and type I IFN receptors.
Studies have shown that drug inhibition of TYK2 by binding to the allosteric activity site in the regulatory domain rather than the active site allosteric in the catalytic domain leads to selective inhibition because the regulatory domain is only present in TYK2, while the active site in the catalytic domain is highly conserved
among members of the JAK superfamily.
Thus, TYK2 allosteric inhibition is more selective than JAK1-3 inhibition and has the potential to limit the toxicity associated with JAK1-3 inhibitors
.
Deucravacitinib is a novel, oral, selective TYK2 inhibitor that blocks IL-12, IL-23, and type I IFN signaling and functional responses, and has been shown to be effective and well tolerated in phase II trials in patients with moderate to severe PsO
.
Clinical trials of deucravacitinib for the treatment of IBD (UC and CD), PsO, PsA and lupus are ongoing
.
Brepocitinib, a TYK2 inhibitor targeting the active site of the TYK2 catalytic domain, is also being evaluated
in IBD patients.
It remains to be seen
whether selective inhibitors of TYK2 can reduce the dimensionality of monoclonal antibody drugs currently used.
Silvio Danese, MD, PhD, Laurent Peyrin-Biroulet, MD, PhD, Selective Tyrosine Kinase 2 Inhibition for Treatment of Inflammatory Bowel Disease: New Hope on the Rise, Inflammatory Bowel Diseases, 2021; , izab135, https://doi.
org/10.
1093/ibd/izab135