-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
For medical professionals only
The use of TAF in patients with relapsed retherapy after discontinuation is well known to mean that HBV recurrence after discontinuation of
nucleoside analogues (NAs) is common
during chronic hepatitis B (CHB) therapy.
Previous studies have shown that the 5-year retreatment rate is 47% in HBeAg-positive CHB patients and 55% in HBeAg-negative CHB patients [1], and HBV recurrence after discontinuation is associated with the risk of disease progression and even death [2].
Therefore, for CHB patients who develop HBV recurrence after discontinuation of the drug, the timing of retherapy and the choice of drug for retreatment are very important
.
Tenofovir propofovir fumarate (TAF), tenofovir fumarate (TDF) and entecavir (ETV) are the first-line antiviral drugs
recommended by domestic and foreign guidelines for the treatment of CHB due to their strong potency and low drug resistance.
However, the efficacy of these three first-line agents after discontinuation and renal safety have not been carefully explored
.
Therefore, the team of Professor Chen Jianhong of Kaohsiung Chang Gung Memorial Hospital in Taiwan designed a retrospective study to evaluate the efficacy and safety of first-line NAs in patients who relapse and retreated after discontinuation of the drug, and pointed out that TAF is one of the regimens for retreatment after relapse after discontinuation of ETV or TDF therapy [3].
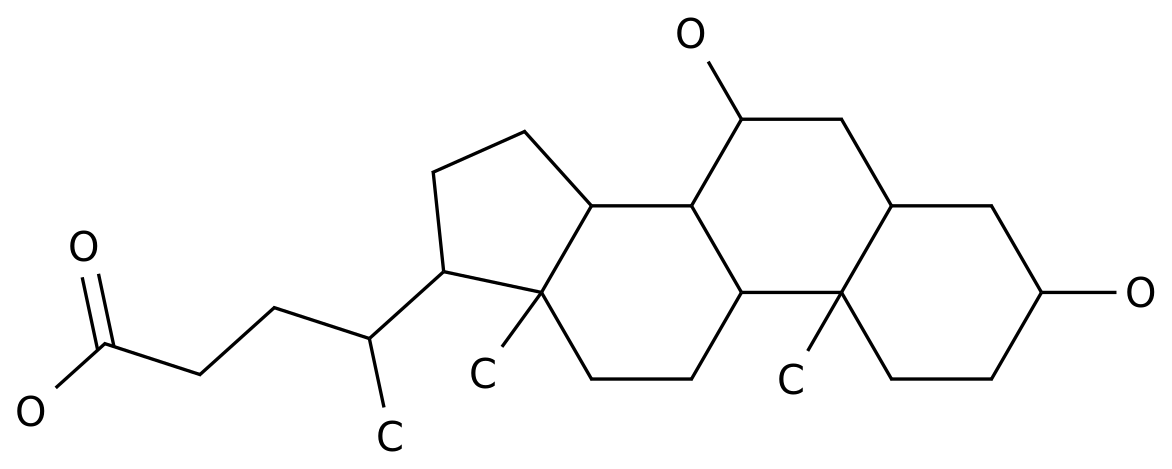
Figure 1 Screenshot of the first page of the paper According to the health plan of Taiwan residents, for HBeAg-positive patients without cirrhosis, the retreatment standard is HBV DNA ≥ 20,000 IU/mL and alanine aminotransferase (ALT) ≥ twice the upper limit of
normal value (ULN).
For HBeAg-negative patients, the criteria for retreatment are 3 months apart, two tests showing ALT≥2×ULN, and HBV DNA ≥ 2,000 IU/mL
.
Finally, this retrospective study included a total of 282 patients
with non-cirrhotic CHB who relapsed after discontinuation of ETV or TDF therapy and met the criteria for retreatment.
These patients chose to receive ETV (n=93), TDF (n=103), or TAF (n=86) for at least 12 months
between 2012 and 2020, on the advice of their physicians and their own wishes.
The primary endpoint of the study was to assess the virological response (HBV DNA<20 IU/mL), estimated glomerular filtration rate (eGFR), and changes in serum HBsAg levels before and after 12 months of treatment in these patients<b22>.
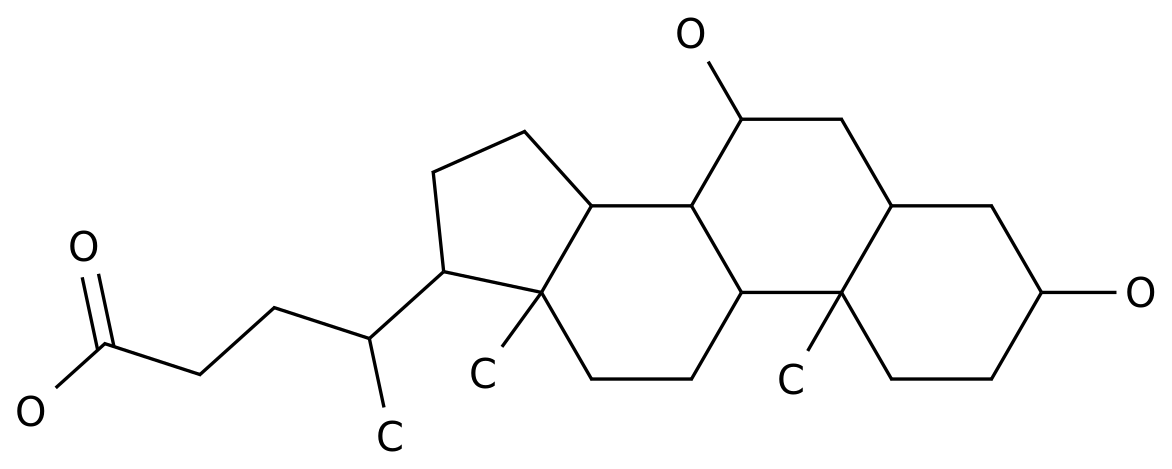
The baseline before retreatment is shown in the table below
.
Fig.
2 In
terms of efficacy, after 12 months of treatment, the virologic response rates of patients in ETV, TDF and TAF were 84.
9% (79/93), 89.
3% (92/103) and 83.
7% (72/86), respectively.
The ALT recurrence rate (ALT≤40 U/L) was 81.
7% (76/93), 74.
7% (77/103) and 84.
9% (73/86),
respectively 。 Although there was no significant difference in virologic response rate (P=0.
495) and ALT repetition rate (P=0.
198) between the three groups overall, at 12 months of treatment, ALT levels in the TDF group were significantly higher than in the ETV group (37.
8±34.
8 U/L vs.
28.
3±19.
3 U/L, P=0.
022) and TAF (37.
8±34.
8 U/L vs.
27.
2±17.
9 U/L, P=0.
015)
。
Figure 3 Changes in ALT levels in the three groups at baseline and 12 months of retreatmentIn order to eliminate the difference in
baseline characteristics of the three groups, the research team used a 1:1:1 propensity score matching (PSM).
。 After PSM, there was a marginal significant difference in ALT recurrence between the three groups (ETV group: 82.
1%, TDF group: 71.
0%, TAF group: 87.
5%, P=0.
057), and there was a significant difference between TDF group and TAF group (P=0.
022).
However, there was still no significant difference in virologic response between the three groups (P=0.
585).
The team performed a multivariate analysis of predictors of virological response after 12 months of retreatment and found that serum HBV DNA (OR: 0.
562, 95% CI: 0.
361-0.
875, P=0.
011) and HBsAg (OR: 0.
498, 95% CI: 0.
253-0.
983, P=) at baseline 0.
045) was an independent predictor
of virologic response in patients with CHB.
In terms of renal safety, there was no significant difference in eGFR from baseline after 12 months of treatment in the three groups (ETV group: 0.
48± 14.
0 mL/min/1.
73m 2, TDF group: −2.
82± 9.
87 mL/min/1.
73m 2, TAF group: 0.
80±9.
30 mL/min/ 1.
73m2,P=0.
120)
。
However, in CHB patients with a baseline eGFR of 60 to 90 mL/min/1.
73 m2, there was a significant difference in eGFR between the three groups (P=0.
008), and renal function improved after12 months of retreatment with TAF and ETV compared with TDF retreatment (TDF group vs.
TAF group, P=0.
011; TDF group vs.
ETV group, P=0.
007, ETV group vs.
TAF group, P=0.
797).
Notably, the research team observed 2 acute kidney injury (AKI) events
only in patients who received TDF retreatment.
Fig.
4 Changes of eGFR in three groups before and after retreatment
In addition, after 12 months of retreatment, serum HBsAg levels decreased by 0.
56±0.
78 log IU/mL, 0.
52±0.
79 log IU/mL and 0.
57±0.
80 log IU/mL, respectively, after 12 months of retreatment, and there was no significant difference between the three groups (P=0.
899).
。 During the entire retreatment period, 278 patients achieved a rapid decrease in serum HBsAg (1≥11 patients with a decrease of 0.
5 log IU/mL ≥ 1.
0 log IU/mL in 111 patients).
Multivariate analysis showed that HBV genotype B, ALT>5×ULN, and higher HBsAg levels at baseline were independently associated with
a decrease in HBsAg ≥ 0.
5 or ≥1.
0 log IU/mL at 12 months of retreatment.
In summary, for patients with non-cirrhotic CHB who developed HBV recurrence after discontinuation of ETV or TDF therapy, most patients achieved a rapid decrease
in virologic response and serum HBsAg after receiving first-line NA for 12 months.
After retreatment, all three groups achieved higher virologic response rates, but patients in the TAF group and ETV group had more advantages in ALT level and renal safety than those in the TDF group at 12 months of treatment
.
Therefore, the research team believes that TAF is one of the options for re-treatment after relapse after discontinuation of
ETV or TDF therapy.
HBV recurrence after discontinuation has attracted much attention
in the treatment as a common clinical problem.
Although this study is a single-center retrospective study with a small sample size, it also provides a meaningful reference for clinical practice, and it is expected that larger prospective randomized controlled studies will be conducted in the future to validate the relevant conclusions to benefit more patients
.
References: [1] Ma TL, Hu TH, Hung CH, et al.
Incidence and predictors of retreatment in chronic hepatitis B patients after discontinuation of entecavir or tenofovir treatment.
PLoS One.
2019 Oct 4; 14(10):e0222221.
[2]Liaw YF.
Hepatitis B Flare After Cessation of Nucleos(t)ide Analogue Therapy in HBeAg-Negative Chronic Hepatitis B:To Retreat or Not to Retreat.
Hepatology.
2021 Feb; 73(2):843-852.
[3]Chiu SM,Chang KC,Hu TH,Hung CH,Wang JH,Lu SN,Chen CH.
Retreatment Efficacy and Renal Safety of Tenofovir Alafenamide,Entecavir,and Tenofovir Disoproxil Fumarate After Entecavir or Tenofovir Cessation.
Dig Dis Sci.
2022 Aug 17.
Past Highlights
1.
From the latest real-world research, look at the current status of first-line treatment of CHB | cutting-edge insights
2.
Speculation about whether CHB patients with normal ALT and HBV DNA positive need antiviral therapy| hot debate
3.
Real-world data in China once again proves that the efficacy and safety of TAF in patients with treatment-naïve and treated CHB | selected by APASL
with AI medical assistant "Xiaozhi"Welcome to "Jizhi Doctor"
This information is for medical and scientific reference only and is not recommended for use in any manner inconsistent with the prescribed information approved in your country.