-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Over the past three decades, a large amount of preclinical and clinical data has shown that almost all targeted anticancer drugs have more or less exerted immunostimulating or immunosuppressive effects, thus affecting the therapeutic effect
These general mechanisms of immunomodulation of targeted anticancer therapy may involve either direct (i.
The ability of targeted anticancer drugs to mediate immunomodulatory effects provides a strong theoretical basis
CDK inhibitors
Cyclin-dependent kinase (CDK) is a family of serine/threonine kinases that regulate cell cycle processes and other cellular processes, including DNA repair, transcription, and metabolism
First, inhibition of CDK4/CDK6 can mediate immunostimulatory effects by promoting exposure to MHC class I molecules on the surface of tumor cells; Secondly, CDK4/CDK6 inhibitors also mediate immunostimulatory effects by promoting the secretion of pro-inflammatory cytokines, such as interferon type III and CC chemokine ligand 5 (CCL5); Finally, various CDK4/CDK6 inhibitors mediate a variety of immunostimulatory effects by interacting directly with immune cells, including (1) activation of nuclear factor 1 (NFATC1) signaling and interleukin-2 (IL-2) secretion by effector T cells by effector T (TEFF) cells, (2) inhibition of immunosuppressive Treg cells by inhibition of DNA methyltransferase 1 (DNMT1), followed by blockade of the cell cycle by CDK inhibitor 1A (CDKN1A).
The immunostimulatory activity of CDK4/CDK6 inhibitors can be offset
In addition, CDK4/CDK6 inhibitors can also be combined with other targeted anti-cancer drugs for better immune stimulation and superior efficacy
KRAS and PI3K inhibitors
Some tumors are driven by acquired mutations or deletions in the KRAS, PI3KCA, or B-Raf protooncogene (BRAF), and phosphatase and tensin homologs (PTEN), which produce constitutive mitotic signals through the signaling pathway of AKT1, MTOR, or MEK
Activation of KRAS and BRAF mutations in malignant cells supports the establishment
On the other hand, loss of antigen presentation, TEFF cell failure, and immunosuppressive cell infiltration
In summary, deregulated KRAS and PI3K signaling mediates powerful carcinogenic effects while facilitating immune evasion
DDR and apoptotic targeted drugs
Certain malignant tumor cells exhibit a high degree of dependence on cDNA damage repair (DDR) mechanisms or strong anti-apoptosis signals, and this dependence has been used to develop targeted anti-cancer drugs
Various FDA-approved and experimental PARP inhibitors have been shown to promote interferon type I secretion in a variety of tumor cells, in some cases, accompanied by the release of T cell chemical attractants, including CXCL10, and paracrine activation in DC, ultimately leading to upregulation of MHC class II molecules and co-stimulatory ligands to support T cell initiation
In addition, PARP inhibitors are associated with PD-L1 upregulation in various cancer cells, regardless of BRCA1/2 status, which can be the result of
ATM has been shown to work with PARP1 to activate a non-classical STING-dependent program that focuses on NF-kB-driven interferon I and IL6 secretion
Another DDR-related kinase ATR has been shown to mediate a potent immunosuppressive effect, so ATR inhibitors not only enhance CGAS signaling and subsequent type I interferon response (involving CCL5 and CXCL10), but also enhance antigen presentation of MHCI-class molecules, ultimately favoring tumor infiltration in DC, TAM repolarization in the direction of immune stimulation, and T-cell-dependent anticancer immunity
DDR-driven BCL2 suppresses the deletion of genes or functions in multiple malignancies of p53, one of the main participants in apoptosis, associated with local immunosuppression
.
Other immunostimulatory effects associated with p53 drug reactivation include (but are not limited to) (1) the downregulation of immunomodulatory cytokines associated with tumor progression, such as IL6; (2) upward adjustment of NKALs; (3) Establish cellular senescence associated with immunostimulated SASP, which facilitates the recruitment and activation
of NK cells, TEFF cells and macrophages.
HER2, EGFR, VEGFA, and TGF-β inhibitors
Over the past two decades, many monoclonal antibodies and TKIs have been developed to target these proteins or their binding partners, and some of these molecules, including HER2-, EGFR- and VEGFA-specific drugs, have been licensed for use in a variety of tumor indications
.
While the safety and efficacy of TGF-β receptor or ligand inhibitors continue to be examined, all of these drugs have been shown to mediate treatment-related immunomodulatory effects
.
HER2-targeted monoclonal antibodies appear to be involved in some degree of CD8+ and CD4+ T cell-dependent HER2-specific immune response, reflecting at least in part the improved presentation of antigen on MHC class I and class II molecules, as well as MYD88-dependent immune stimulation, ultimately leading to increased DC antigen processing and presentation
.
A variety of immunotherapeutic agents, including DC-based vaccines, TLR2 agonists, recombinant IL21, and PD-L1 blockers, can be used to amplify the efficacy of HER2-targeted monoclonal antibodies while stimulating strong anti-tumor immunity
.
Various EGFR-targeted preparations improve MHCI antigen presentation in cancer cells and favor DC uptake of tumor material and the ability to
excite T cells and promote NK cell activation without additional immune stimulation signals.
In addition, multiple TKIs targeting EGFR effectively reduce PD-L1 expression in NSCLC cells, reflecting their ability to
block NF-kB and IL6 signaling.
Consistent with this immunomodulatory profile, TME exposed to EGFR-targeted drugs in NSCLC showed increased abundance of DC and CD8+ Tesff cells, as well as depletion
of Treg cells and M2 TAM.
VEGFA monoclonal antibodies, as well as drugs targeting VEGFA receptors, mediate immunostimulation effects independent of ADCC and ADCP, largely reflecting the key role
of VEGFA in establishing cancer-associated immunosuppression.
For example, VEGFA signaling is directly involved in Treg cell expansion and co-inhibition of receptor expression, including PD-1 of CD8+ CTL
.
In addition, transcriptome analysis showed that VEGFA levels in biopsy tissues and preclinical models of breast cancer and colorectal cancer were negatively correlated
with CD8+ CTL invasion features.
Finally, in a mouse model of ovarian cancer, the accumulation of immunosuppressive cells, including TAM, is associated
with resistance to VEGFA-targeted antibodies.
TGF-β is best known for its ability to upregulate PD-L1 in malignant and myeloid cells in TME, promotes PD-1 expression in T cells, and facilitates the expansion of Treg cells and MDSCs, ultimately leading to local and systemic immunosuppression
.
In addition, TGF-β is closely related to the establishment of immune rejection, a process by which cancer cells bind to cancer-associated fibroblasts to prevent invasion of tumors by immune effector cells
.
Inhibition of TGF-β or its receptors resolves immune rejection and improves antigen presentation in malignant cells, ultimately producing a potent anti-tumor immune response that works in conjunction with ICIs to eliminate tumors and establish a protective immune memory
.
Furthermore, although TGF-β plays a central role in the establishment of tumor-associated immunosuppression, a combination of one or more ICI protocols is required to fully exploit the clinical potential
of TGF-β inhibitors.
In this case, the order of treatment may be a key determinant of
success.
In fact, by supporting matrix metal peptidase 9 (MMP9)-driven PD-L1 lysis, pre-TGF-β inhibition appears to promote resistance
to PD1 blockers at least to some extent.
Conversely, once PD-1 resistance is acquired, the administration of TGF-β inhibitors produces a powerful therapeutic effect
.
other
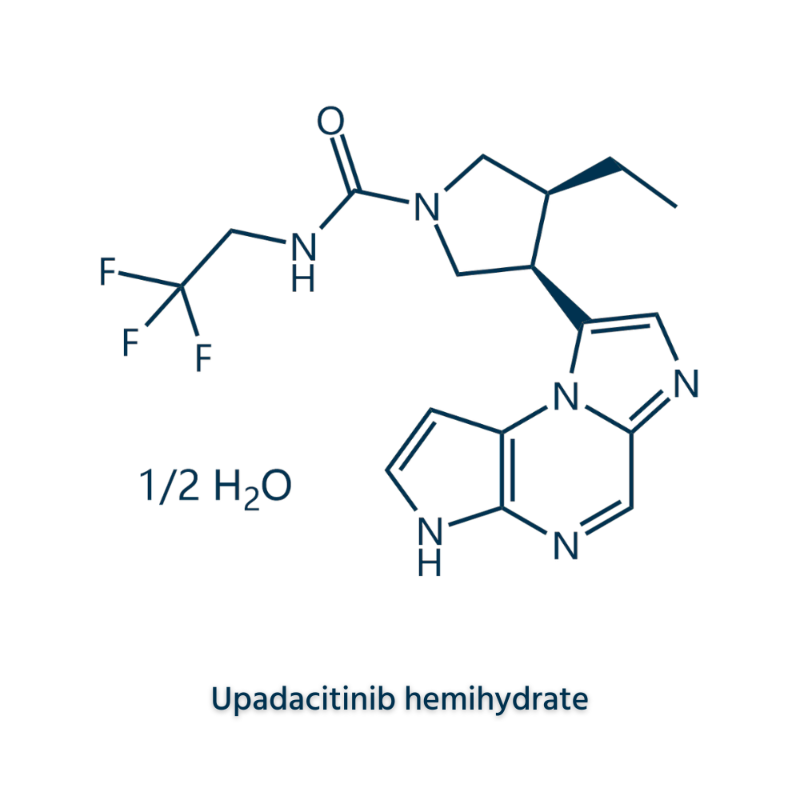
The list of targeted anticancer drugs that are approved or are being developed is growing, including the relatively selective ALK receptor tyrosine kinase (ALK); AXL receptor tyrosine kinase (AXL); Bruton tyrosine kinase (BTK); zeste homologous 2 enhancer (EZH2); Histone deacetylase (HDAC); Isocitrate dehydrogenase 1 (IDH1); Janus kinase 1 (JAK1); MET protooncogene, receptor tyrosine kinase (MET); RET protooncogene (RET); ROS proto-oncogene 1, receptor tyrosine kinase (ROS1); Smooth curl receptors (SMO) and exportin 1 (XPO1) inhibitors; Monoclonal antibodies specific to CD20, CD22, CD33, CD52, CD58; IL2 receptor sub α (CD25); IL3 receptor sub α (IL3RA); Tumor-associated calcium signal transducer 2 (TROP2); and multi-target TKIs
.
Interestingly, most of these clinically used drugs mediate at least some degree of immunomodulation, providing a theoretical basis
for the design of combination regimens involving ICIs.
Outlook and outstanding issues
Targeted anticancer drugs mediate powerful immunomodulatory effects, and they either favor a positive immune response or counteract negative immunosuppressive pathways, so the combination of targeted anticancer drugs with ICIs and other immunotherapy strategies shows promising applications
.
However, the biological basis of research on immunomodulation of targeted antitumor drugs is just beginning, and there are still some problems to be solved
in this regard.
First, what is the actual specificity of these drugs for their molecular targets? Imatinib was designed to target the kinase domain of ABL1 to inhibit constitutive signaling in the BCR-ABL1 chimera, and it was found that it inhibited a variety of clinically relevant kinases
.
Along a similar lines, abemaciclib is thought to inhibit CDK4/CDK6, but has been shown to target other CDKs as well as CDK-independent kinases
.
Thus, although in some cases immunomodulation targeting antitumor therapies is clearly derived from targeted effects, in many other cases it stems from alternative (often featureless) other participating molecules
.
Especially when immune cells are directly involved, it is urgent to identify these alternative targets
.
Second, what is the exact molecular mechanism at work when immunomodulation actually stems from the inhibition of expected molecular targets in malignant cells? There are no specifically designed targeted anticancer drugs to mediate immunomodulatory effects, which means that the various proteins that support tumorigenesis also affect the ability of tumor cells to
transmit immunostimuli or immunosuppressive signals.
For example, active CDK4/CDK6 signaling limits DNMT1's ability to drive the expression of endogenous retroviral elements, which would otherwise promote type III IFN secretion, a pathway that can function
through clinically used CDK4/CDK6 inhibitors.
Accurately identifying similar pathways induced by targeted anticancer drugs will provide a variety of additional targets that can be used to enhance a clinically meaningful tumor-specific immune response
.
This is especially important when the immunomodulatory activity of a drug is multifunctional and involves beneficial and harmful effects that can be exploited
differently by targeting downstream signal transducers.
Third, what are the key factors in the differences in immunomodulatory effects mediated by certain targeted anticancer drugs in a given environment? Most drugs are associated with immunostimulation and immunosuppressive effects, depending on the specific experimental scenario
.
However, while in some cases the source of this difference is obvious, in many other cases the underlying mechanisms remain unclear
.
In the latter case, experimental variables such as drug concentration, precise media composition, and timing can have an unexpected effect on
biological results.
In addition, potentially overlooked and/or difficult to control heterogeneous, epigenetic, or metabolic sources may have key effects, especially in vivo
.
Further research is needed on the effect of tumor heterogeneity on the immunomodulatory effects of
targeted anticancer drugs.
Fourth, how can conventional chemotherapy and radiotherapy be used to maximize the ability to target antineoplastic drugs to drive clinically meaningful tumor-specific immune responses? It is clear (at least some) that targeted anticancer drugs are promising combination partners for a variety of immunotherapies, including ICIs
.
However, whether the efficacy of these combination therapies can be further enhanced by conventional chemotherapy or RT has not been fully studied
.
In summary, only by gaining an in-depth understanding of the molecular pathways in which targeted antineoplastic mediates clinically relevant immunomodulation and envisioning multimodal treatment regimens with good immunostimulating activity can the number of
tumor indications for clinical benefit from targeted anticancer therapies be further expanded.
References:
1.
Immunomodulation by targeted anticancer agents.
Cancer Cell.
2020 Dec 17; S1535-6108(20)30601-2.