-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Only for medical professionals to read and refer to
the expert summary! Clear and easy to understand
The detection rate of intestinal metaplasia varies significantly around the world, and a 2020 meta-analysis of the American AGA Society [1] shows that the three regions with the highest detection rate of intestinal metaplasia in the world are South America, East Asia and Eastern Europe, and these three regions are also the highest incidence of
gastric cancer in the world.
A single-center prospective cohort study [2] with a follow-up of 15 years found that after eradication of Helicobacter pylori (Hp), the cumulative incidence of gastric cancer was 1.
5% if intestinal metaplasia was absent in the gastric mucosa, and if intestinal metaplasia was present in the antrum, The cumulative incidence of gastric cancer in patients reached 5.
3%.
If intestinal metaplasia is present in both the stomach body and antrum, the cumulative incidence of gastric cancer is as high as 9.
8%.
The results of this study showed that the presence of intestinal metaplasia significantly increased the risk of
carcinogenesis in patients.
Even after eradication of Hp, intestinal metaplasia remains an independent risk factor
for the development of gastric cancer.
A cohort study from a region with a low incidence of gastric cancer in Western countries [3], with a follow-up of more than 330,000 cases and an average follow-up of 10 years, found that the risk of gastric cancer in patients with superficial gastritis, atrophic gastritis, intestinal metaplasia and dysplasia increased by 2.
6 times, 4.
5 times, 6.
2 times and 10.
9 times
, respectively, compared with normal gastric mucosa.
The annual incidence of gastric cancer in patients with intestinal metaplasia is also different in different regions, and it is 0.
25%
in Western Europe.
Another study from East Asia [4] showed that the annual incidence of gastric cancer in East Asian intestinal metaplasia patients is as high as 10%.
As early as 1998, some scholars proposed that intestinal metaplasia is an irreversible point
of gastric mucosal lesions.
Studies believe that after eradicating Hp, the incidence of gastric cancer can be significantly reduced, gastric mucosal atrophy can be improved, but intestinal metaplasia is difficult to reverse
.
But in 1990, Professor Correa, who proposed the Correa model, discovered the spontaneous reversal of enteric survival
.
His team followed 1422 residents of high-risk areas in Colombia for an average of 5.
1 years [5] and found that gastric mucosal lesions not only evolved from low to high grades, but also from high to low grades, but spontaneous reversal was masked because the rate of migration from low to high levels was greater than the rate of migration from high to low grades
.
For example, the rate of change in the transition from intestinal metaplasia to atrophy is 5.
4%, but the rate of intestinal metaplasia rising from atrophy to intestinal metaplasia is 5.
8%, so the reversal of intestinal metaplasia to atrophy is masked
.
This study[5] also found that the age of 40 is a very critical time point
.
After age 40, the rate of change from low to high level progression further increases, while the rate of high level to low level evolution decreases further, making spontaneous reversals difficult to detect
.
A 2018 study [6] with a 10-year follow-up found that although the reversal of intestinal metaplasia was slow after eradication of Hp, 33.
9% of patients with antrum and 44.
4% of patients with gastric body parts had reversal of intestinal metaplasia during the follow-up period 5-10 years after eradication of Hp
.
Inspired by this study, several more studies were published
in 2021 to support this conclusion.
A study of 380 patients followed for 12 years [7] showed that after eradication of Hp, the improvement rate of gastric antrum and gastric systemic metaplasia reached 61.
1% and 37.
9% endoscopically, respectively, and 70% and 76.
1%
under pathology.
The study estimated that it would take 4-6 years for antral and gastric body metaplasia to be observed endoscopically and 3-5 years for improvement to be observed under microscopy after eradication of Hp
.
This shows that as long as the follow-up time is long enough, it can still be observed that intestinal metaplasia reverses after eradication of Hp, but its reversal is later and slower
than the reversal of atrophy.
Another study[8] from the United States was a prospective cohort study that looked at 800 Hispanic patients and followed 356 of them for 20 years
.
This study showed that the reversal rate of intestinal metaplasia was about 18%-20%, and that eradication of Hp could reduce the progression rate
of precancerous lesions in the entire stomach cancer.
Another retrospective cohort study [9] from Thailand that followed 2025 patients for two years found that the reversal rate of intestinal metaplasia could reach 57.
3%.
For patients with Hp infection, the reversal rate of intestinal metaplasia is relatively low, 39.
4%, while in patients without Hp infection, the reversal rate of intestinal metaplasia can be as high as 60.
4%, which once again confirms that intestinal metaplasia can be reversed, and the reversal rate of intestinal metaplasia is related
to the state of Hp infection.
In fact, some drugs can help reverse intestinal metaplasia
.
Celecoxib: An RCT study of celecoxib [10], randomized patients who still had intestinal metaplasia one year after successful Hp eradication into two groups, one receiving usual care as a control and the other receiving celecoxib
.
Follow-up results found that celecoxib can make the reversal rate of intestinal metaplasia reach 44.
3% to 51.
7%.
Morodan is similar, with a 2016 multicenter RCT study [11] using Morodan
to treat patients with intestinal metaplasia for six months in the experimental group of 130 patients and 66 patients in the control group, It was found that Morodan's reversal rate of intestinal metaplasia could reach 23%.
The control group was the folic acid treatment group, and the intestinal metaplasia reversal rate in this group was also 13.
6%.
Lamb Stomach Lamb Stomach
Extract VitaminB 12 Granules/Capsules, which we often call lamb stomach, conducted a phase IV clinical trial in 2012 in a randomized, double-blind, placebo-controlled experimental design for patients with HV-negative chronic atrophic gastritis.
There are 17 centers in the country participating, and the treatment course of lamb stomach is half a year, and finally the calibration biopsy is used to observe the pathological changes to evaluate the efficacy
of lamb's stomach.
It was found that the reversal rate of lamb's stomach to intestine exceeded 50%, and the reversal rate of atrophy exceeded 20%.
In the first half of this year, China also issued the "Expert Guidance on the Diagnosis and Treatment of Chronic Atrophic Gastritis and the Clinical Application of Lamb Gastric Extract Vitamin B 12" [12], advocating that patients with severe intestinal metaplasia can be treated with lamb's stomach.
A study [13] proved that the reversal rate of intestinal metaplasia reached more than 50%, whether it was the initial treatment of lamb's stomach or the salvage treatment of celecoxib, and the overall intestinal metaplasia reversal rate of the combination therapy of the two could reach 85.
93
%.
At enrollment, 21 patients with enterocytosis were accompanied by low-grade intraepithelial neoplasia, and after 6 months of initial treatment with lamb's stomach, 19 of them had low-grade intraepithelial neoplasia disappeared
.
This study also found that the effect of lamb stomach treatment is closely related to the OLGIM stage in patients with intestinal metaplasia, and the benefit is more obvious in patients with high stage of OLGIM, which also indicates that the more severe the intestinal metaplasia lesions, the easier it is to benefit
from the treatment of lamb's stomach and celecoxib.
How to do a good job in the diagnosis, treatment and detection of intestinal metaplasia?
For patients with intestinal metaplasia, we must first evaluate the condition, mainly based on pathological assessment, and guide patients to eliminate the corresponding risks on the basis of evaluation, including detecting and eradicating Hp infection, avoiding long-term use of PPI, quitting smoking, avoiding eating pickled and smoked foods, and actively intervening in bile reflux
.
The patient can then be stratified
according to pathology to become cancerous.
For high-risk patients, including patients with stage III and IV intestinal metaplasia, as well as patients with incomplete and type III intestinal metaplasia, small doses of drugs can be given for reversal therapy
.
Patients who fail to reverse therapy should be followed annually
.
For patients with stage 0-II OLGIM, or patients with complete type I/II intestinal metaplasia, patients with low-risk intestinal metaplasia can be considered to be treated with or without drug therapy and only follow-up
.
For this subset of patients, follow-up should be followed every three years, and if there is a family history of gastric cancer, the interval between follow-up visits should be shortened to one to two years
.
Professor Shi Yongquan, an audit expert
Where to see more clinical knowledge of digestive liver disease? Come to the "Doctor's Station" and take a look 👇
at the references:
[1] Gawron AJ, Shah SC, Altayar O, Davitkov P, Morgan D, Turner K, Mustafa RA.
AGA Technical Review on Gastric Intestinal Metaplasia-Natural History and Clinical Outcomes.
Gastroenterology.
2020 Feb; 158(3):705-731.
e5.
doi: 10.
1053/j.
gastro.
2019.
12.
001.
Epub 2019 Dec 6.
PMID: 31816300; PMCID: PMC7375032.
[2]Gastrointests Endosc.
2016[3]Song H, Ekheden IG, Zheng Z, Ericsson J, Nyrén O, Ye W.
Incidence of gastric cancer among patients with gastric precancerous lesions: observational cohort study in a low risk Western population.
BMJ.
2015 Jul 27; 351:h3867.
doi: 10.
1136/bmj.
h3867.
Erratum in: BMJ.
2015; 351:h4134.
PMID: 26215280; PMCID: PMC4516137.
[4]Huang RJ, Choi AY, Truong CD, Yeh MM, Hwang JH.
Diagnosis and Management of Gastric Intestinal Metaplasia: Current Status and Future Directions.
Gut Liver.
2019 Nov 15; 13(6):596-603.
doi: 10.
5009/gnl19181.
PMID: 31394893; PMCID: PMC6860040.
[5]Cancer Res,1990.
[6]Aliment Pharmacol Ther,2018.
[7] Dig Dis Sci,2021.
[8]Gastroenterology,2021.
[9]PLoS One,2021.
[10]Helicobacter,2013.
[11]Chin J Integr Med,2016.
[12] CHEN Hongmei, CHEN Min.
"Expert guidance on the diagnosis and treatment of chronic atrophic gastritis and the clinical application of lamb gastric extract vitamin B12", Chinese Journal of Digestion, Vol.
42, No.
9, September 2022 Chin J Dig, September 2022, Vol ,41,No.
9[13]Word J Clin Cases,2021.
the expert summary! Clear and easy to understand
What is intestinal metaplasia?
Intestinal metaplasia refers to the replacement of gastric mucosal epithelial cells by intestinal epithelial cells, that is, epithelial cells similar to the small intestine or large intestine mucosa appear in the gastric mucosa, which is a common lesion of the gastric mucosa and is seen in a variety of chronic gastric diseases
.
At the recently held 2022 Asia-Pacific Digestive Week Disease Conference and the 22nd National Digestive Disease Academic Conference of the Chinese Medical Association, Professor Shi Yongquan from Xijing Hospital of Air Force Military Medical University shared the reversal therapy of intestinal metaplasia for us.
The detection rate of intestinal metaplasia is closely related to the incidence of gastric cancer
The detection rate of intestinal metaplasia varies significantly around the world, and a 2020 meta-analysis of the American AGA Society [1] shows that the three regions with the highest detection rate of intestinal metaplasia in the world are South America, East Asia and Eastern Europe, and these three regions are also the highest incidence of
gastric cancer in the world.
A single-center prospective cohort study [2] with a follow-up of 15 years found that after eradication of Helicobacter pylori (Hp), the cumulative incidence of gastric cancer was 1.
5% if intestinal metaplasia was absent in the gastric mucosa, and if intestinal metaplasia was present in the antrum, The cumulative incidence of gastric cancer in patients reached 5.
3%.
If intestinal metaplasia is present in both the stomach body and antrum, the cumulative incidence of gastric cancer is as high as 9.
8%.
The results of this study showed that the presence of intestinal metaplasia significantly increased the risk of
carcinogenesis in patients.
Even after eradication of Hp, intestinal metaplasia remains an independent risk factor
for the development of gastric cancer.
Risk of carcinogenesis in different gastric mucosal states
A cohort study from a region with a low incidence of gastric cancer in Western countries [3], with a follow-up of more than 330,000 cases and an average follow-up of 10 years, found that the risk of gastric cancer in patients with superficial gastritis, atrophic gastritis, intestinal metaplasia and dysplasia increased by 2.
6 times, 4.
5 times, 6.
2 times and 10.
9 times
, respectively, compared with normal gastric mucosa.
The annual incidence of gastric cancer in patients with intestinal metaplasia is also different in different regions, and it is 0.
25%
in Western Europe.
Another study from East Asia [4] showed that the annual incidence of gastric cancer in East Asian intestinal metaplasia patients is as high as 10%.
Is intestinal metaplasia really an irreversible point of gastric mucosal lesions?
As early as 1998, some scholars proposed that intestinal metaplasia is an irreversible point
of gastric mucosal lesions.
Studies believe that after eradicating Hp, the incidence of gastric cancer can be significantly reduced, gastric mucosal atrophy can be improved, but intestinal metaplasia is difficult to reverse
.
But in 1990, Professor Correa, who proposed the Correa model, discovered the spontaneous reversal of enteric survival
.
His team followed 1422 residents of high-risk areas in Colombia for an average of 5.
1 years [5] and found that gastric mucosal lesions not only evolved from low to high grades, but also from high to low grades, but spontaneous reversal was masked because the rate of migration from low to high levels was greater than the rate of migration from high to low grades
.
For example, the rate of change in the transition from intestinal metaplasia to atrophy is 5.
4%, but the rate of intestinal metaplasia rising from atrophy to intestinal metaplasia is 5.
8%, so the reversal of intestinal metaplasia to atrophy is masked
.
This study[5] also found that the age of 40 is a very critical time point
.
After age 40, the rate of change from low to high level progression further increases, while the rate of high level to low level evolution decreases further, making spontaneous reversals difficult to detect
.
How to reverse intestinal metaplasia? Eradicate Hp
A 2018 study [6] with a 10-year follow-up found that although the reversal of intestinal metaplasia was slow after eradication of Hp, 33.
9% of patients with antrum and 44.
4% of patients with gastric body parts had reversal of intestinal metaplasia during the follow-up period 5-10 years after eradication of Hp
.
Inspired by this study, several more studies were published
in 2021 to support this conclusion.
A study of 380 patients followed for 12 years [7] showed that after eradication of Hp, the improvement rate of gastric antrum and gastric systemic metaplasia reached 61.
1% and 37.
9% endoscopically, respectively, and 70% and 76.
1%
under pathology.
The study estimated that it would take 4-6 years for antral and gastric body metaplasia to be observed endoscopically and 3-5 years for improvement to be observed under microscopy after eradication of Hp
.
This shows that as long as the follow-up time is long enough, it can still be observed that intestinal metaplasia reverses after eradication of Hp, but its reversal is later and slower
than the reversal of atrophy.
Another study[8] from the United States was a prospective cohort study that looked at 800 Hispanic patients and followed 356 of them for 20 years
.
This study showed that the reversal rate of intestinal metaplasia was about 18%-20%, and that eradication of Hp could reduce the progression rate
of precancerous lesions in the entire stomach cancer.
Another retrospective cohort study [9] from Thailand that followed 2025 patients for two years found that the reversal rate of intestinal metaplasia could reach 57.
3%.
For patients with Hp infection, the reversal rate of intestinal metaplasia is relatively low, 39.
4%, while in patients without Hp infection, the reversal rate of intestinal metaplasia can be as high as 60.
4%, which once again confirms that intestinal metaplasia can be reversed, and the reversal rate of intestinal metaplasia is related
to the state of Hp infection.
Drug intervention reverses intestinal metaplasia
In fact, some drugs can help reverse intestinal metaplasia
.
Celecoxib: An RCT study of celecoxib [10], randomized patients who still had intestinal metaplasia one year after successful Hp eradication into two groups, one receiving usual care as a control and the other receiving celecoxib
.
Follow-up results found that celecoxib can make the reversal rate of intestinal metaplasia reach 44.
3% to 51.
7%.
Morodan is similar, with a 2016 multicenter RCT study [11] using Morodan
to treat patients with intestinal metaplasia for six months in the experimental group of 130 patients and 66 patients in the control group, It was found that Morodan's reversal rate of intestinal metaplasia could reach 23%.
The control group was the folic acid treatment group, and the intestinal metaplasia reversal rate in this group was also 13.
6%.
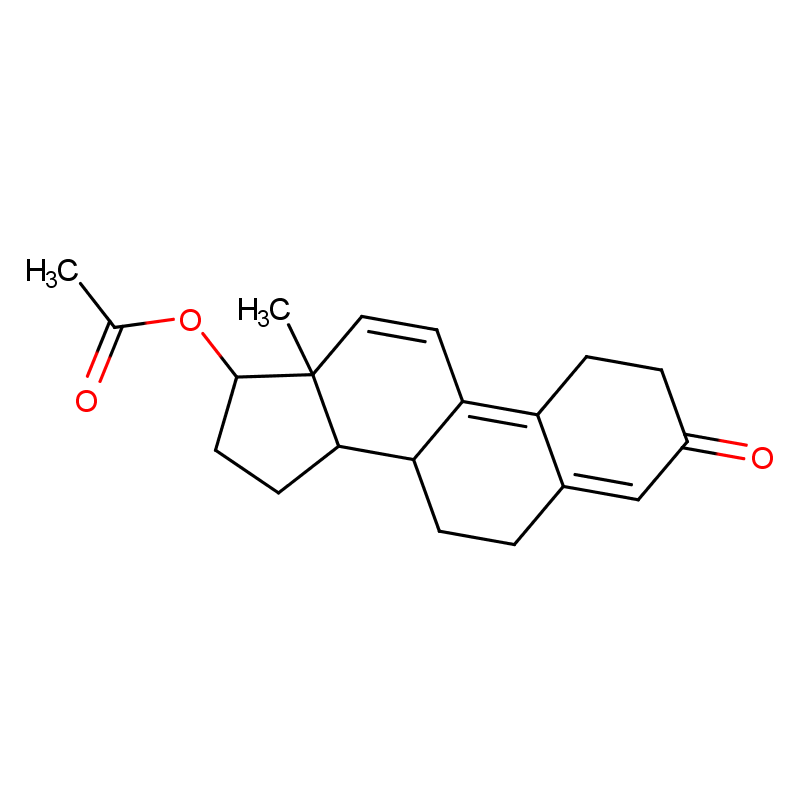
Lamb Stomach Lamb Stomach
Extract VitaminB 12 Granules/Capsules, which we often call lamb stomach, conducted a phase IV clinical trial in 2012 in a randomized, double-blind, placebo-controlled experimental design for patients with HV-negative chronic atrophic gastritis.
There are 17 centers in the country participating, and the treatment course of lamb stomach is half a year, and finally the calibration biopsy is used to observe the pathological changes to evaluate the efficacy
of lamb's stomach.
It was found that the reversal rate of lamb's stomach to intestine exceeded 50%, and the reversal rate of atrophy exceeded 20%.
In the first half of this year, China also issued the "Expert Guidance on the Diagnosis and Treatment of Chronic Atrophic Gastritis and the Clinical Application of Lamb Gastric Extract Vitamin B 12" [12], advocating that patients with severe intestinal metaplasia can be treated with lamb's stomach.
A study [13] proved that the reversal rate of intestinal metaplasia reached more than 50%, whether it was the initial treatment of lamb's stomach or the salvage treatment of celecoxib, and the overall intestinal metaplasia reversal rate of the combination therapy of the two could reach 85.
93
%.
At enrollment, 21 patients with enterocytosis were accompanied by low-grade intraepithelial neoplasia, and after 6 months of initial treatment with lamb's stomach, 19 of them had low-grade intraepithelial neoplasia disappeared
.
This study also found that the effect of lamb stomach treatment is closely related to the OLGIM stage in patients with intestinal metaplasia, and the benefit is more obvious in patients with high stage of OLGIM, which also indicates that the more severe the intestinal metaplasia lesions, the easier it is to benefit
from the treatment of lamb's stomach and celecoxib.
summary
How to do a good job in the diagnosis, treatment and detection of intestinal metaplasia?
For patients with intestinal metaplasia, we must first evaluate the condition, mainly based on pathological assessment, and guide patients to eliminate the corresponding risks on the basis of evaluation, including detecting and eradicating Hp infection, avoiding long-term use of PPI, quitting smoking, avoiding eating pickled and smoked foods, and actively intervening in bile reflux
.
The patient can then be stratified
according to pathology to become cancerous.
For high-risk patients, including patients with stage III and IV intestinal metaplasia, as well as patients with incomplete and type III intestinal metaplasia, small doses of drugs can be given for reversal therapy
.
Patients who fail to reverse therapy should be followed annually
.
For patients with stage 0-II OLGIM, or patients with complete type I/II intestinal metaplasia, patients with low-risk intestinal metaplasia can be considered to be treated with or without drug therapy and only follow-up
.
For this subset of patients, follow-up should be followed every three years, and if there is a family history of gastric cancer, the interval between follow-up visits should be shortened to one to two years
.
Professor Shi Yongquan, an audit expert
- Deputy Director of the Department of Gastroenterology, Xijing Hospital, Air Force Military Medical University
- Chief physician, professor, doctoral supervisor
- Vice Chairman of Internal Medicine Branch of Chinese Medical Association
- Member and Secretary of the Gastroenterology Branch of the Chinese Medical Association
- Leader of the Digestive Oncology Collaborative Group of the Chinese Medical Association
Where to see more clinical knowledge of digestive liver disease? Come to the "Doctor's Station" and take a look 👇
at the references:
[1] Gawron AJ, Shah SC, Altayar O, Davitkov P, Morgan D, Turner K, Mustafa RA.
AGA Technical Review on Gastric Intestinal Metaplasia-Natural History and Clinical Outcomes.
Gastroenterology.
2020 Feb; 158(3):705-731.
e5.
doi: 10.
1053/j.
gastro.
2019.
12.
001.
Epub 2019 Dec 6.
PMID: 31816300; PMCID: PMC7375032.
[2]Gastrointests Endosc.
2016[3]Song H, Ekheden IG, Zheng Z, Ericsson J, Nyrén O, Ye W.
Incidence of gastric cancer among patients with gastric precancerous lesions: observational cohort study in a low risk Western population.
BMJ.
2015 Jul 27; 351:h3867.
doi: 10.
1136/bmj.
h3867.
Erratum in: BMJ.
2015; 351:h4134.
PMID: 26215280; PMCID: PMC4516137.
[4]Huang RJ, Choi AY, Truong CD, Yeh MM, Hwang JH.
Diagnosis and Management of Gastric Intestinal Metaplasia: Current Status and Future Directions.
Gut Liver.
2019 Nov 15; 13(6):596-603.
doi: 10.
5009/gnl19181.
PMID: 31394893; PMCID: PMC6860040.
[5]Cancer Res,1990.
[6]Aliment Pharmacol Ther,2018.
[7] Dig Dis Sci,2021.
[8]Gastroenterology,2021.
[9]PLoS One,2021.
[10]Helicobacter,2013.
[11]Chin J Integr Med,2016.
[12] CHEN Hongmei, CHEN Min.
"Expert guidance on the diagnosis and treatment of chronic atrophic gastritis and the clinical application of lamb gastric extract vitamin B12", Chinese Journal of Digestion, Vol.
42, No.
9, September 2022 Chin J Dig, September 2022, Vol ,41,No.
9[13]Word J Clin Cases,2021.