-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
In recent years, with the vigorous development of immunotherapy in the field of oncology, hematological malignancies have also entered the era of immunotherapy.
Compared with traditional drugs, immunotherapy can significantly improve the survival rate and remission rate of patients
.
But what are the similarities and differences in the adverse events associated with immunotherapy compared with traditional chemotherapy drugs? At the 2021 China Conference on Oncology (CCO) held online from April 14 to 17, 2022, Professor Mei Heng from Union Hospital Affiliated to Huazhong University of Science and Technology gave the title of "Coagulation events in hematological tumor immunotherapy".
It focuses on the identification and management of coagulation events in three aspects: anti-inflammatory antibodies, immune checkpoint inhibitors and CAR-T cell therapy
.
The development of immunotherapy from the first use of "Colley's mixed toxin" by William Coley in 1981 to treat a variety of cancers to the first FDA approval of CD19-targeted CAR-T cell therapy for tumor treatment in 2014.
There are a growing number of categories, including antibody therapy, adoptive cell therapy, immune checkpoint inhibitors, oncolytic viruses, and tumor vaccines
.
Professor Mei Heng said that immunotherapy drugs have brought great hope to patients with hematological tumors, which can significantly improve the remission rate and survival rate
.
Bispecific antibodies More than 84 bispecific antibodies have been used in clinical trials.
The results of two trials published in the Lancet Oncology in 2015 and the New England Journal in 2017 showed that 43% of B Cellular acute lymphoblastic leukemia (B-ALL) patients achieved complete remission/complete remission with partial hematologic recovery (CR/CRh) after using bispecific antibody drugs, and the median overall survival (OS) was 6.
1 months; 45% of patients who relapsed after allogeneic hematopoietic stem cell transplantation (allo-HSCT) achieved CR/CRh after two cycles of bispecific antibody therapy, with a median OS of 8.
5 months
.
Professor Mei Heng summarized the adverse events of the above two clinical studies.
The adverse reactions of patients receiving bispecific antibody treatment were mainly fever, headache, febrile neutropenia and neurological complications.
Hematology-related toxic events are cytokine release syndrome (CRS), which leads to abnormal coagulation function, but the severity is not as severe as that of CAR-T cell therapy.
Therefore, the coagulation disorder directly caused by bispecific antibody therapy is relatively rare, and attention should be paid to it.
One is bispecific antibody drug-associated CRS
.
Immune checkpoint inhibitors The common targets of immune checkpoint inhibitors (ICIs) are CTLA-4, PD-1 and PD-L1
.
For ICI-related bleeding events, from the analysis of 19 large ICI clinical studies, it can be found that the incidence of ICI-related hematological toxicity events is about 3.
6% (63 cases), the most common of which is idiopathic thrombocytopenic purpura (ITP; 18 cases); another meta-analysis of 80 clinical trials showed that the incidence of ITP accounted for 27% (36/135) of hematological toxicity events
.
In the above two studies, hemophagocytic syndrome (HLH) accounted for 7.
4% and 11% of ICI-related hematologic toxicity events, respectively, and the response rates to immunosuppression were 50% and 60%, respectively
.
In 2019, WHO reported 168 ICI-related safety reports.
The incidence of coagulation events was low, but the incidence of ITP and HLH was high: PD-1 inhibitor users had the highest incidence of ITP, and CTLA-4 inhibitor users had the highest incidence of HLH.
highest rate
.
Professor Mei Heng concluded from these findings that although the incidence of ICI-related coagulation disorders is low, ITP accounts for the highest proportion of hematological toxicity events, which needs our attention
.
Professor Mei Heng also emphasized that we should pay attention to the occurrence of HLH.
Although HLH is not a category of coagulation diseases, HLH patients have a high risk of bleeding, especially those who use CTLA-4 inhibitors, and HLH patients are not immune to immunosuppressive therapy.
Still a good response
.
For ICI-related thrombotic events, a study was published in the journal Blood in 2021.
The results showed that the cumulative incidence of venous thromboembolism (VTE) was 5%-8% and 12.
9% at a median follow-up of 6, 8.
5, and 14.
6 months, respectively.
At a median follow-up of 8.
5 months, the cumulative incidence of arterial thromboembolism (ATE) was 1.
8%
.
However, the study further analyzed factors related to thrombosis risk, and the results showed that thrombosis risk was associated with previous VTE history, shorter OS and progression-free survival (PFS), and was associated with ICI type, tumor type and stage, and PD-L1 expression level.
Factors are irrelevant
.
Regarding the mechanism of ICI-induced coagulation dysfunction, previous studies have shown that ICI can induce the activation of immune cells and cause the release of cytokines, leading to the activation of the coagulation system and platelets and inhibiting the fibrinolytic system; mouse models have demonstrated that PD-1 inhibition has The role of promoting atherosclerosis and increasing the risk of thrombosis
.
In addition, factors such as other failed treatment prior to ICI therapy, advanced disease stage, and tumor types with higher risk of VTE and ATE such as non-small cell lung cancer are all prothrombotic risk factors
.
As for the treatment of ITP, the Chinese Guidelines for the Diagnosis and Treatment of Primary Immune Thrombocytopenia in Adults (2020 Edition) recommend first-line pulse dexamethasone therapy; high-dose gamma globulin therapy is recommended for patients with bleeding; When globulin is ineffective, thrombopoietin-promoting drugs such as eltrombopag and recombinant human thrombopoietin are recommended
.
For the treatment of HLH, the opinion on the management of adult hemophagocytic syndrome published in the journal Blood in 2019 suggests that HLH caused by immunotherapy needs to correct the high cytokine status to avoid the progression of HLH, and etoposide should be used as soon as possible when symptoms do not improve
.
For the treatment of thromboembolic events, the Guidelines for the Prevention and Treatment of Tumor-related Venous Thromboembolism (2019 Edition) pointed out that there is no clear evidence that ICI is a risk factor for thrombosis, and prophylactic anticoagulation is not recommended; If there is no contraindication, anticoagulation therapy should be given immediately, including unfractionated heparin and low molecular weight heparin
.
Professor Mei Heng summarized the treatment of coagulation events with immune checkpoint inhibitors as follows: 1.
ITP recommends high-dose dexamethasone 40mg/d × 4 days, orally or intravenously; or prednisone 1mg/kg/d (maximum Dosage 80mg/d), pay attention to monitoring blood pressure and blood sugar levels during treatment, and pay attention to preventing infection and peptic ulcer bleeding.
Patients with high-dose IVIG pulse therapy are recommended to use thrombopoietic drugs when hormones and or IVMG are ineffective: recombinant human platelet production 2.
HLH (1) Induction and remission therapy for HLH, aiming at correcting the state of high cytokines and controlling the progression of HLH; (2) Etiological treatment, controlling other inducing factors such as primary disease and infection
.
In order to prevent the recurrence of HLH, the treatment plan is mainly based on HLH-94 and the revised HLH-2004 plan, giving hormones and tocilizumab
.
After 48 hours, the symptoms do not improve, and etoposide can be added.
3.
Thrombosis There is no clear evidence that ICI is a risk factor for thrombosis
.
Therefore, it is not recommended to stop ICI before prophylactic anticoagulation or acute thrombosis occurs before the start of ICl; use the Khorana score to assess the risk of thrombosis in patients after diagnosis of VTE and PE, and immediately anticoagulation if there are no contraindications
.
(1) Unfractionated heparin: intravenous administration, loading dose of 80U/kg, and infusion of 18U/kg/h
.
The treatment goal is to make APTT reach 2.
0-2.
5 times the normal value (2) Low molecular weight heparin: 80-100U/kg, subcutaneous injection, qd (3) Warfarin: 2.
5-5 mg orally, once a day; adjusted dose INR in 2-3, CAR-T cell therapy for long-term treatment and prevention of relapse Prof.
Mei Heng finally focused on the coagulation events related to CAR-T cell therapy
.
CAR-T cell therapy is a very promising treatment method in tumor treatment.
More than 1,500 studies have been registered with NCT, of which Chinese studies account for more than 1/3
.
The world's first child receiving CAR-T cell therapy has achieved 10-year tumor-free survival
.
Although the efficacy of CAR-T cell therapy is obvious to all, its adverse reactions involve multiple systems and are more prone to life-threatening situations.
Therefore, early identification of CAR-T-related adverse reactions is a key issue to be solved in the promotion of CAR-T therapy
.
The NCCN guidelines (2022 edition) provide a summary of CRS, neurotoxicity events, and HLH in CAR-T therapy, but the guidelines do not specifically mention CAR-T-related coagulation events
.
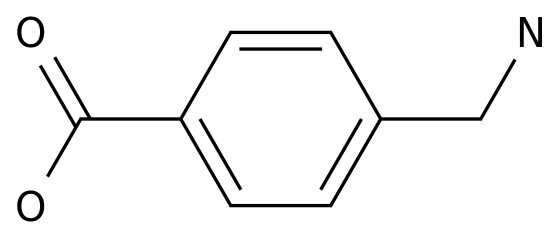
Based on this, the team of Professor Hu Yu, President of Wuhan Union Medical College Hospital, and the team of Professor Han Weidong of the Chinese People's Liberation Army Hospital jointly compiled a Chinese expert consensus on coagulation disorders related to CAR-T cell therapy, and made a consensus on CAR-T-related coagulation disorders (CARAC).
) to give relevant definitions, as shown in Figure 1
.
Professor Mei Heng said that from the previous CAR-T-related clinical trials, the incidence of CARAC is not low, ranging from 51% to 56.
6%.
Factors related to the occurrence of CARAC include: the number of previous treatments; the expansion of CAR-T cells extent; free fibrinogen and baseline platelet levels; occurrence of CRS
.
The incidence of abnormal coagulation index in patients with severe CRS was significantly increased, and the onset time point and recovery time point of abnormal coagulation index were after CRS; inflammatory factors interleukin-6 (IL-6), interferon γ (IFN- γ), C-reactive protein (CRP), and ferritin were all positively correlated with coagulation markers
.
Figure 1 The most prominent and life-threatening clinical feature of CARAC is disseminated intravascular coagulation (DIC)
.
A study published in Annals of Hematology in 2019 showed that the incidence of DIC in CARAC patients is about 14%-50%, and the specific clinical manifestations include ecchymosis, jaundice, hypotension, dyspnea, shock and neurological abnormalities
.
In addition, Professor Mei Heng also said that bleeding is another main feature of CARAC.
From previous studies, 19.
6% of CARAC patients will have clinically significant bleeding, but the incidence of thrombosis is lower than that of bleeding events, ranging from 6.
3% to 8.
8%.
%
.
The main cause of CARAC pathogenesis is CRS.
The cytokine storm caused by CRS leads to the increase of inflammatory factors, mainly IL-6, and causes the imbalance of inflammation and coagulation.
The core mechanism of CARAC pathogenesis is vascular endothelial injury.
Previous studies have shown that patients with severe CRS Serum VWF, TF, FX, FXII and other serological indexes related to vascular endothelial injury were higher than those in mild CRS patients
.
For the clinical diagnosis of CARAC, according to the consensus of Chinese experts on coagulation disorders related to CAR-T cell therapy, Professor Mei Heng said that it is necessary to clarify the basic conditions of the patient, including: whether there are high-risk factors, such as high tumor burden, CAR-T cells High-speed amplification, high CRS level; determine the degree of increase in cytokines such as IL-6, and determine whether CRS exists
.
Then determine whether the patient's clinical manifestations are in line with CARAC
.
Finally, the laboratory-related test results were clarified, including the degree of thrombocytopenia, changes in coagulation indexes and fibrinolytic indexes, especially fibrinolytic indexes such as FDP and D-dimer, which had significant changes in CARAC patients
.
In the end, Professor Mei Heng emphasized that once a patient begins to experience abnormal coagulation indicators, according to the guidelines, the Chinese Disseminated Intravascular Coagulation (CDSS) or the International Society of Thrombosis and Hemostasis (ISTH) scoring system should be used to score DIC every day
.
For the treatment of CARAC, according to the consensus of Chinese experts on coagulation disorders related to CAR-T cell therapy, Professor Mei Heng emphasized that the treatment principles of early identification, accurate assessment, removal of incentives, and stratified intervention should be adhered to, from the control of CRS to replacement therapy.
, anticoagulation and antifibrinolysis to ensure the life safety of patients
.
Summary Professor Mei Heng said that clinicians should grasp the similarities and differences between immunotherapy-related coagulation events and coagulation events caused by other causes.
For example, the therapeutic effect of CAR-T therapy-related DIC plasma exchange is better than that of shock-related DIC.
The reason is that the DIC of the former is mainly caused by cytokine storm
.
In the field of hematological tumors, immunotherapy is undoubtedly a very important treatment method, but the coagulation events related to cell therapy cannot be ignored
.
Professor Mei Heng Professor, Chief Physician, Doctoral Supervisor of Union Hospital Affiliated to Tongji Medical College, Huazhong University of Science and Technology, Young Changjiang Scholar of the Ministry of Education, winner of Outstanding Youth in Hubei Province, Vice Chairman of the Youth Committee of the Chinese Society of Hematology, Deputy Head of the Thrombosis and Hemostasis Group Member of the Standing Committee of the Biotherapy Committee of China Research Hospitals, Vice Chairman of the Hematology Branch of the Hubei Provincial Clinical Oncology Society 1 key research and development sub-project of the Ministry, 4 items of the National Natural Science Foundation of China, 2 authorized invention patents in 30 SCI articles in the first communication such as Lancet Oncology, Lancet Haematology, CCR, JBC, etc.
, and 1 item won the second prize of the National Science and Technology Progress Award.
"Diagnosis and Efficacy Criteria" and "Williams Hematology" CAR-T results were rated as the 2019 BEST OF ASH Review: Quinta Typesetting: Wenting Execution: Wenting pokes "read the original text", we make progress together