-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
In the early 20th century, Nobel Prize winner Dr.
Karl Landsteiner discovered the ABO blood group in humans
.
Scientific accumulation over the past century has found that blood type is not only related to safe blood transfusion, but also affects human immunity and disease infection [1]
.
But little known is that ABO blood type is actually inextricably linked with human microbes [2]
.
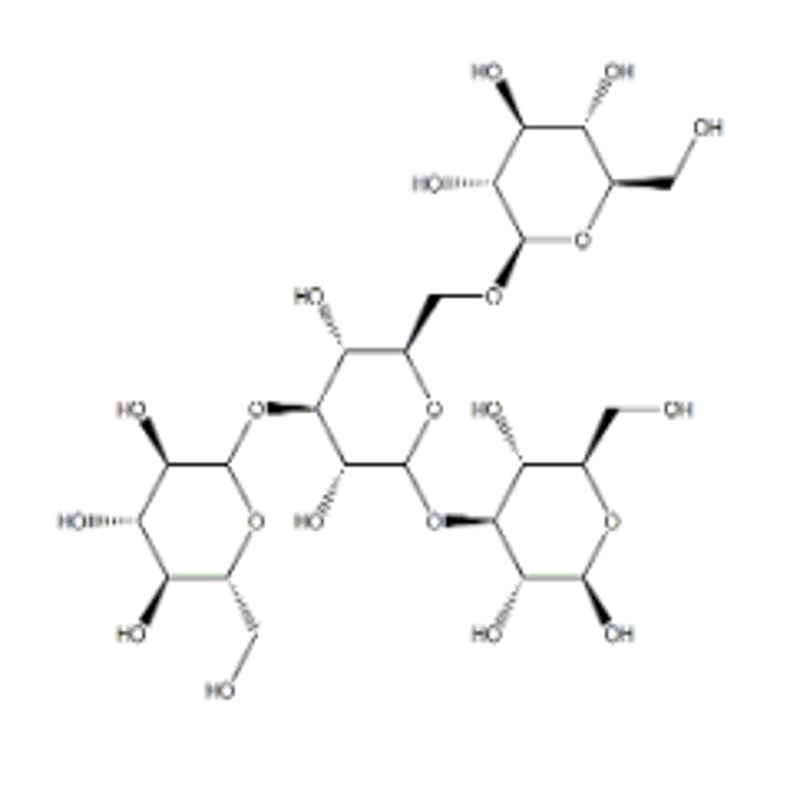
Schematic representation of the ABO antigen on the surface of human erythrocytes
.
Quoted from Reference [1] In January last year, a study published in the journal Nature Genetics reported the association between human ABO blood type and intestinal microbial composition [3]
.
Based on the German population, the scientists found that the interaction of the ABO and FUT2 genes has a certain effect on the abundance of Bacteroides and Faecalibacterium in the gut
.
However, this finding was limited to the German population, and the signal did not reach Study-wide significance and was not validated by other populations
.
The study used 16S rRNA gene amplification and sequencing to identify the flora.
This technology has limited resolution of the flora and its identification performance is not as good as the more reliable shotgun metagenomic sequencing
.
On February 3 this year, "Nature Genetics" published two back-to-back association studies between the host and gut microbes based on large populations, and at the same time verified the effect of the interaction of ABO and FUT2 genes on the composition of gut microbes
.
The first study was based on a Finnish cohort of about 6,000 people and was completed by an international team led by Michael Inouye from several laboratories in Melbourne, Cambridge, Helsinki and San Diego [4].
Chinese researcher Dr.
Tan Youwen is the independent first in this study.
Author (currently working at Shenzhen BGI)
.
Screenshot of the Finnish cohort paper front page Another study is based on a Dutch cohort of about 7700 people, completed by a European team led by Alexandra Zhernakova and Serena Sanna [5]
.
It is worth noting that both studies used shotgun metagenomic sequencing to identify microbiota, and were completed in a single center, reducing experimental and technical errors between multiple centers, and their accuracy was comparable to the previously mentioned German study.
Compared with , there has been a great improvement
.
Looking at the three studies, it is not difficult to find that the associated genetic loci and microbes reported in these studies are not the same
.
Two independent loci located on the ABO locus were associated with the abundance of Faecalibacterium and Bacteroides in a German population study
.
In the Finnish population, however, two other sites on the ABO gene were associated with the abundance of Faecalicatena lactaris and Collinsella
.
In the Dutch population, loci on the ABO gene were in turn associated with the abundance of Bifidobacterium, Collinsella, lactose and galactose degradation pathways
.
Although the associations found in the three studies are reflected in different genetic loci and microbial species, these studies consistently reveal that the interaction between the ABO and FUT2 genes affects the composition of the microbiota
.
The antigen controlled by ABO gene is a polysaccharide substance that can be decomposed and utilized by specific bacteria; the expression of ABO antigen in mucosal cells is controlled by FUT2 gene [6]
.
People with the genotype FUT2 rs601338:AG/AA can secrete ABO antigens in mucosal cells, which is called "secretory type"
.
People with genotype FUT2 rs601338:GG do not secrete ABO antigens in mucosal cells and are called "non-secreting"
.
In "secretory" people, the intestinal mucosa can secrete ABO antigens, which promote the growth of certain bacteria
.
About 85% of people in the world are FUT2-secreting, and another 15% are non-secreting
.
These findings advance the understanding of host-microbe interactions and provide new ideas for precise intervention in the gut microbiome in the future
.
"Nature Genetics" introduced these two studies in the cover form.
Why can these specific bacteria decompose complex polysaccharides of human origin? Because the metabolic function of bacteria requires specific biological enzymes, and these enzymes are regulated by genetic codes
.
The researchers focused on the existing bacterial genomes and found that F.
lactaris has genes for decomposing ABO antigens and mucosal polysaccharides, and in vitro culture experiments also observed that the bacteria can grow in a medium with porcine mucosa as a single carbon source [4, 7]
.
These evidences fully support the inference that ABO antigens can act as bacterial nutrients
.
Since dietary fiber intake affects the abundance of mucosal degrading bacteria, including Collinsella, which is associated with ABO genes [8], studies in Finnish and Dutch populations also analyzed the effect of diet on ABO gene-microbiota associations influence
.
Consistent with previous studies, the abundance of Collinsella and other mucosa-degrading bacteria in the gut was negatively correlated with dietary fiber intake in the Finnish population
.
However, in A/B/AB "secreting" people, the abundance of F.
lactaris did not correlate with dietary fiber intake; in non-A/B/AB "secreting" people, the abundance of F.
lactaris correlated with There is a positive correlation with dietary fiber intake
.
In the Dutch population, the researchers found no effect of dietary fiber intake on the association of ABO genes with bacteria
.
The dietary data in this study were obtained 4 years earlier than the gut microbiota sampling time, which is underrepresented and may be the reason why no association was found in the Dutch study
.
Effects of genetic variation and dietary fiber intake on intestinal F.
lactaris and Collinsella
.
The picture comes from reference [4] In summary, the effects of ABO and FUT2 genes on gut microbes have been confirmed in German, Finnish and Dutch populations
.
Can these patterns be reproduced in other populations? Previously, a Chinese research team based on about 1,500 Chinese young people also revealed the effect of ABO genes on gut microbes [9]
.
As the study sample size was smaller than the European population, the association signal was weaker
.
As the sample size of the study increases, it is likely that more similar findings will be found in studies in China and other non-European populations
.
In addition, these two studies also verified the effects of LCT sites and dairy products on Bifidobacterium
.
The large populations in Finland and the Netherlands started to build many years ago, and it is expected that domestic scientists will also build similar large-scale studies
.
References: 1.
Bayne-Jones, S.
, DR.
KARL LANDSTEINER NOBEL PRIZE LAUREATE IN MEDICINE, 1930.
Science, 1931.
73(1901): p.
599-604.
2.
Arnolds, KL, CG Martin, and CA Lozupone, Blood type and the microbiome- untangling a complex relationship with lessons from pathogens.
Current Opinion in Microbiology, 2020.
56: p.
59-66.
3.
Rühlemann, MC, et al.
, Genome-wide association study in 8,956 German individuals identifies influence of ABO histo-blood groups on gut microbiome.
Nature Genetics, 2021.
53(2): p.
147-155.
4.
Qin, Y.
, et al.
, Combined effects of host genetics and diet on human gut microbiota and incident disease in a single population cohort.
Nature Genetics, 2022.
5.
Lopera-Maya, EA, et al.
, Effect of host genetics on the gut microbiome in 7,738 participants of the Dutch Microbiome Project.
Nature Genetics, 2022.
6.
Wacklin, P.
, et al.
,Secretor genotype (FUT2 gene) is strongly associated with the composition of Bifidobacteria in the human intestine.
PloS one, 2011.
6(5).
7.
Leitch, EC, et al.
, Selective colonization of insoluble substrates by human faecal bacteria.
Environ Microbiol, 2007.
9(3): p.
667-79.
8.
Desai, MS, et al.
, A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility.
Cell, 2016.
167(5): p .
1339-1353.
e21.
9.
Liu, X.
, et al.
, Mendelian randomization analyses support causal relationships between blood metabolites and the gut microbiome.
Nature Genetics, 2022.
54(1): p.
52-61.
Tan YouwenEnviron Microbiol, 2007.
9(3): p.
667-79.
8.
Desai, MS, et al.
, A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility.
Cell, 2016.
167(5): p.
1339-1353.
e21.
9.
Liu, X.
, et al.
, Mendelian randomization analyses support causal relationships between blood metabolites and the gut microbiome.
Nature Genetics, 2022.
54(1): p.
52-61.
This paper Author: Qin YouwenEnviron Microbiol, 2007.
9(3): p.
667-79.
8.
Desai, MS, et al.
, A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility.
Cell, 2016.
167(5): p.
1339-1353.
e21.
9.
Liu, X.
, et al.
, Mendelian randomization analyses support causal relationships between blood metabolites and the gut microbiome.
Nature Genetics, 2022.
54(1): p.
52-61.
This paper Author: Qin Youwen